Introduction
Pain in the testis or scrotum can be a distressing symptom that may indicate an underlying medical condition. It is important to assess and diagnose the cause of this pain to provide appropriate treatment and prevent any potential complications. This guide aims to provide a step-by-step approach to diagnosing and managing pain in the testis or scrotum.
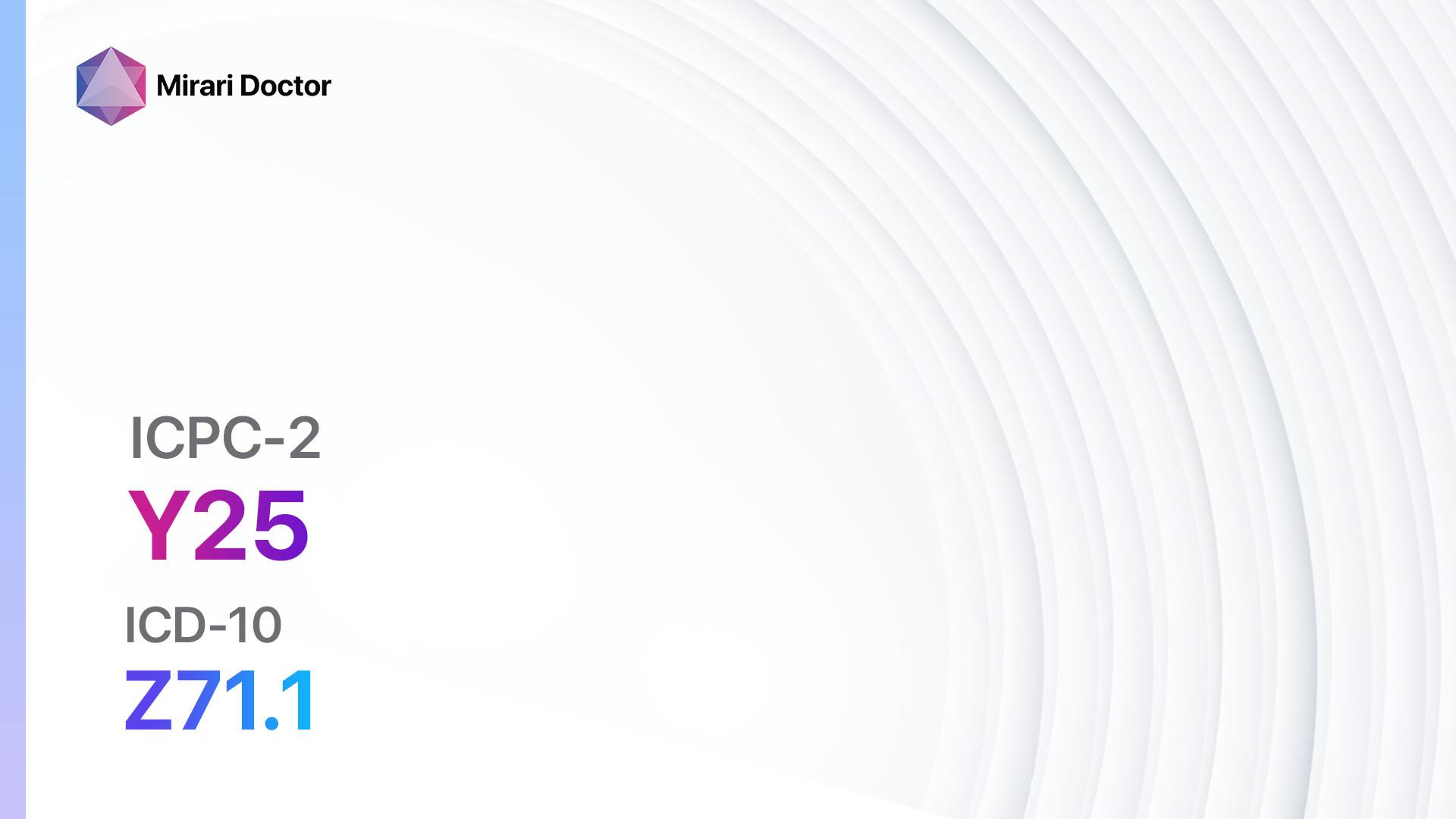
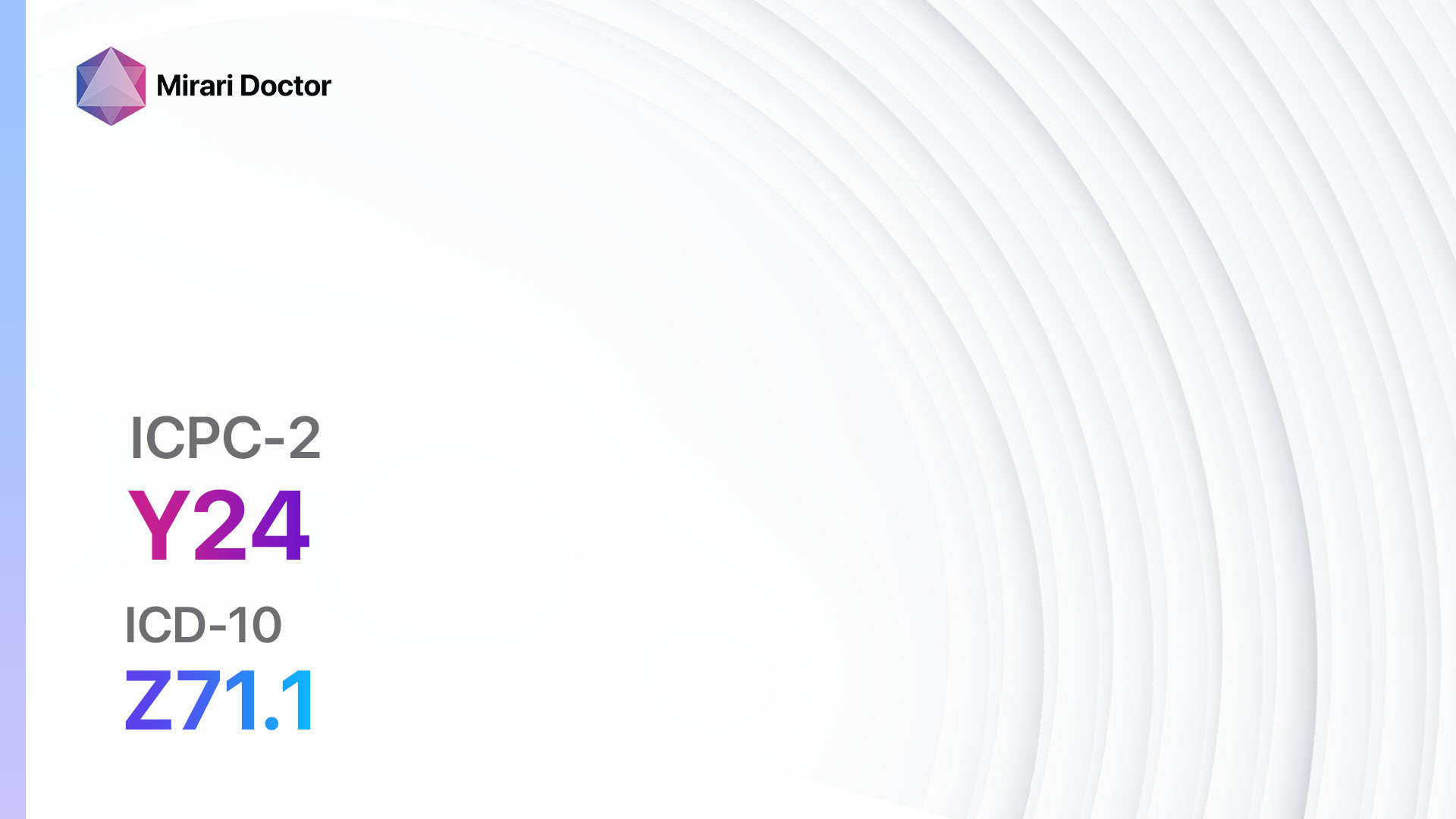
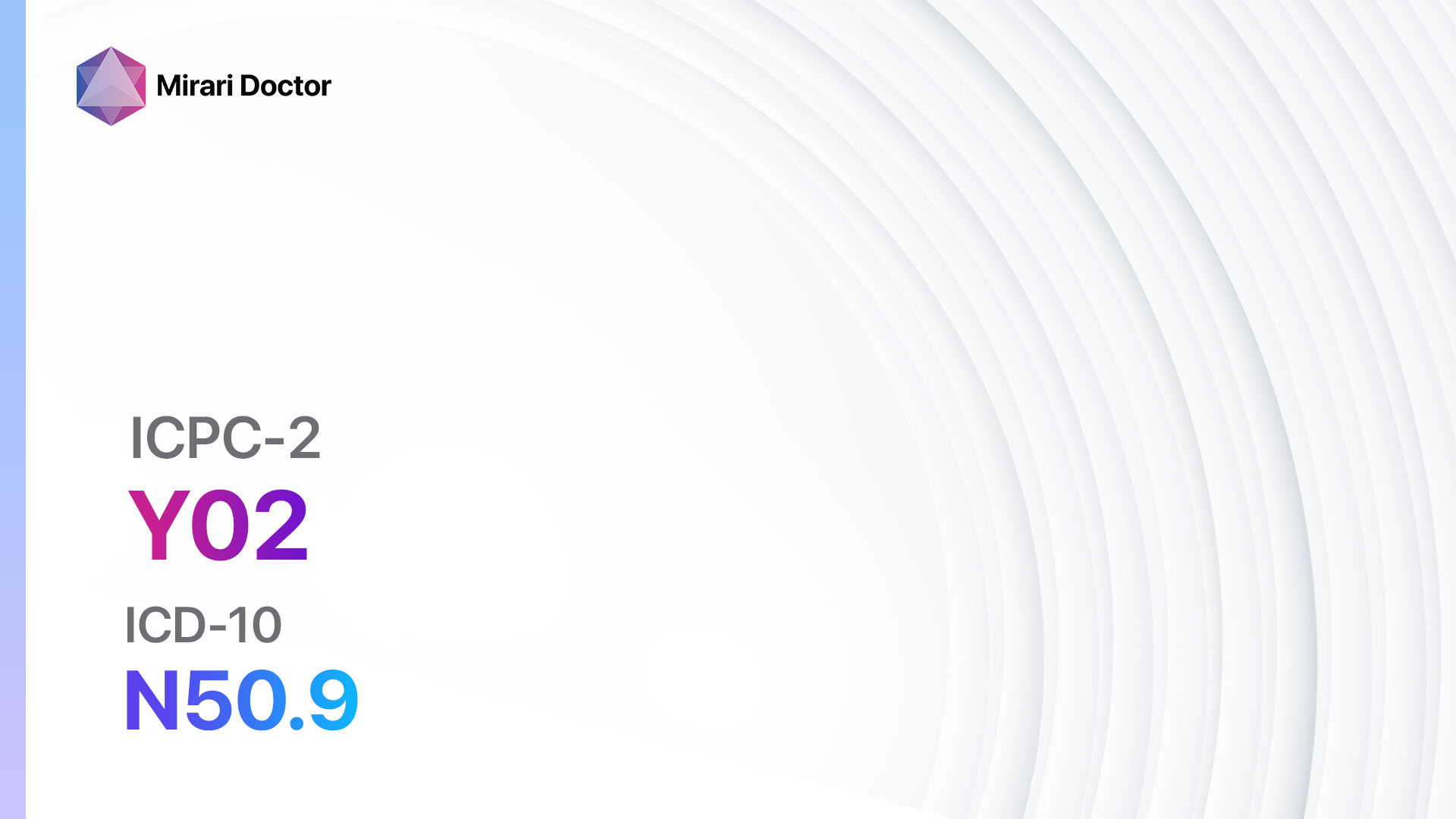
Codes
- ICPC-2 Code: Y02 Pain in testis/scrotum
- ICD-10 Code: N50.9 Disorder of male genital organs, unspecified
Symptoms
- Testicular pain: A dull, achy, or sharp pain in one or both testicles.[1]
- Scrotal pain: Pain in the scrotum, which may be localized or radiate to the groin, abdomen, or back.[2]
Causes
- Testicular torsion: Twisting of the spermatic cord, cutting off the blood supply to the testicle.[3]
- Epididymitis: Inflammation of the epididymis, often due to infection.[4]
- Orchitis: Inflammation of the testicle, usually caused by a viral or bacterial infection.[5]
- Testicular trauma: Injury to the testicle or scrotum.[6]
- Inguinal hernia: Protrusion of abdominal contents into the inguinal canal.[7]
- Varicocele: Enlarged veins in the scrotum.[8]
- Testicular cancer: Abnormal growth of cells in the testicle.[9]
- Kidney stones: Hard deposits that form in the kidneys and may cause referred pain to the testis or scrotum.[10]
Diagnostic Steps
Medical History
- Obtain a detailed medical history, including the onset, duration, and characteristics of the pain.
- Ask about any associated symptoms, such as swelling, redness, urinary symptoms, or history of trauma.
- Inquire about any recent infections, sexual activity, or risk factors for testicular cancer.
Physical Examination
- Perform a thorough physical examination, including inspection, palpation, and auscultation of the testes, scrotum, and inguinal area.
- Assess for any swelling, tenderness, or masses in the testicles or scrotum.
- Check for any signs of infection, such as redness, warmth, or discharge.
- Examine the abdomen and groin for any hernias or masses.
Laboratory Tests
- Complete blood count (CBC): To assess for signs of infection or inflammation.
- Urinalysis: To evaluate for urinary tract infection or kidney stones.
- Sexually transmitted infection (STI) testing: If there is a suspicion of STI-related epididymitis or orchitis.
- Tumor markers: Such as alpha-fetoprotein (AFP) and beta-human chorionic gonadotropin (ß-hCG), if testicular cancer is suspected.
Diagnostic Imaging
- Ultrasound: To evaluate the testicles, scrotum, and inguinal area for any abnormalities, such as testicular torsion, epididymitis, or masses.
- X-ray: If there is a concern for trauma or presence of kidney stones.
- Magnetic resonance imaging (MRI) or computed tomography (CT) scan: If further evaluation of the abdomen or pelvis is required.
Other Tests
- Uroflowmetry: To assess the flow rate and pattern of urine, especially if there are urinary symptoms.
- Cystoscopy: If there is a suspicion of bladder or urethral pathology.
- Vasography: To evaluate the patency of the vas deferens in cases of suspected infertility or vasectomy-related pain.
Follow-up and Patient Education
- Schedule a follow-up appointment to review the results of diagnostic tests and discuss the diagnosis and treatment options.
- Provide patient education on the importance of testicular self-examination, safe sexual practices, and when to seek medical attention for recurrent or worsening symptoms.
Possible Interventions
Traditional Interventions
Medications:
Top 5 drugs for pain in testis/scrotum:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) (e.g., Ibuprofen, Naproxen):
- Cost: Generic versions can be $3-$20/month.
- Contraindications: History of gastrointestinal bleeding, renal impairment, or hypersensitivity to NSAIDs.
- Side effects: Upset stomach, heartburn, headache.
- Severe side effects: Gastrointestinal bleeding, kidney damage, allergic reactions.
- Drug interactions: Anticoagulants, corticosteroids, selective serotonin reuptake inhibitors (SSRIs).
- Warning: Prolonged use may increase the risk of cardiovascular events.
- Antibiotics (e.g., Ciprofloxacin, Doxycycline):
- Cost: Generic versions can be $4-$50/month.
- Contraindications: Hypersensitivity to antibiotics or history of tendon rupture (fluoroquinolones).
- Side effects: Upset stomach, diarrhea, rash.
- Severe side effects: Allergic reactions, tendon rupture (fluoroquinolones).
- Drug interactions: Antacids, iron supplements, warfarin.
- Warning: Take antibiotics as prescribed and complete the full course of treatment.
- Analgesics (e.g., Acetaminophen):
- Cost: Generic versions can be $3-$10/month.
- Contraindications: Severe liver disease or hypersensitivity to acetaminophen.
- Side effects: Rare at therapeutic doses.
- Severe side effects: Liver toxicity (with high doses or chronic use).
- Drug interactions: Warfarin, alcohol.
- Warning: Do not exceed the recommended dose. Avoid alcohol consumption.
- Alpha-blockers (e.g., Tamsulosin):
- Cost: Generic versions can be $10-$30/month.
- Contraindications: Hypersensitivity to alpha-blockers or history of orthostatic hypotension.
- Side effects: Dizziness, headache, abnormal ejaculation.
- Severe side effects: Orthostatic hypotension, priapism.
- Drug interactions: Other alpha-blockers, nitrates.
- Warning: Take medication as directed, especially with regards to dosing and timing.
- Antifungal medication (e.g., Fluconazole):
- Cost: Generic versions can be $10-$50/month.
- Contraindications: Hypersensitivity to antifungal medications.
- Side effects: Upset stomach, headache, rash.
- Severe side effects: Severe allergic reactions, liver toxicity.
- Drug interactions: Warfarin, oral hypoglycemics.
- Warning: Take medication as prescribed and complete the full course of treatment.
Alternative Drugs: – Muscle relaxants (e.g., Cyclobenzaprine): Useful for relieving muscle spasms in cases of testicular trauma or referred pain from the back or abdomen. – Tricyclic antidepressants (e.g., Amitriptyline): May be beneficial for neuropathic pain or chronic testicular pain not responding to other treatments. – Antianxiety medications (e.g., Diazepam): Can help reduce anxiety and muscle tension that may contribute to testicular pain. – Topical analgesics (e.g., Lidocaine gel): Provide localized pain relief for conditions such as epididymitis or trauma. – Antidepressants (e.g., Sertraline): May be beneficial in cases of chronic testicular pain with a significant psychological component.
Surgical Procedures:
- Orchiopexy: Surgical fixation of the testicle in cases of testicular torsion.
- Varicocelectomy: Surgical removal or ligation of the enlarged veins in the scrotum (varicocele).
- Herniorrhaphy: Surgical repair of an inguinal hernia.
- Testicular biopsy: Removal of a small sample of testicular tissue for further evaluation in cases of suspected testicular cancer.
- Orchiectomy: Surgical removal of the testicle in cases of testicular cancer or severe testicular pain with no other treatment options.
Alternative Interventions
- Acupuncture: May help reduce pain, improve blood flow, and promote relaxation. Cost: $60-$120 per session.
- Herbal supplements: Some herbs, such as saw palmetto or stinging nettle, may have anti-inflammatory or analgesic properties. Cost: Varies depending on the specific supplement.
- Heat or cold therapy: Applying heat or cold packs to the affected area can help alleviate pain and reduce inflammation. Cost: Varies depending on the type of therapy used.
- Physical therapy: Pelvic floor exercises, stretching, and manual therapy techniques may help relieve muscle tension and improve symptoms. Cost: $50-$150 per session.
- Mind-body techniques: Stress reduction techniques, such as meditation, deep breathing exercises, or yoga, may help manage pain and improve overall well-being. Cost: Varies depending on the specific technique and location.
Lifestyle Interventions
- Scrotal support: Wearing supportive underwear or using a scrotal support device can help alleviate pain and provide comfort. Cost: $10-$50 per item.
- Avoidance of triggers: Identifying and avoiding activities or positions that worsen the pain can help manage symptoms.
- Stress management: Engaging in stress-reducing activities, such as exercise, relaxation techniques, or counseling, may help improve symptoms. Cost: Varies depending on the specific activity or service used.
- Healthy lifestyle habits: Maintaining a healthy diet, regular exercise, and adequate hydration can promote overall well-being and potentially reduce pain. Cost: Varies depending on individual choices and preferences.
- Sexual activity modification: Adjusting sexual positions or avoiding activities that exacerbate pain may be beneficial. Cost: None.
It is important to note that the cost ranges provided are approximate and may vary depending on the location and availability of the interventions.
Mirari Cold Plasma Alternative Intervention
Understanding Mirari Cold Plasma
- Safe and Non-Invasive Treatment: Mirari Cold Plasma is a safe and non-invasive treatment option for various skin conditions. It does not require incisions, minimizing the risk of scarring, bleeding, or tissue damage.
- Efficient Extraction of Foreign Bodies: Mirari Cold Plasma facilitates the removal of foreign bodies from the skin by degrading and dissociating organic matter, allowing easier access and extraction.
- Pain Reduction and Comfort: Mirari Cold Plasma has a local analgesic effect, providing pain relief during the treatment, making it more comfortable for the patient.
- Reduced Risk of Infection: Mirari Cold Plasma has antimicrobial properties, effectively killing bacteria and reducing the risk of infection.
- Accelerated Healing and Minimal Scarring: Mirari Cold Plasma stimulates wound healing and tissue regeneration, reducing healing time and minimizing the formation of scars.
Mirari Cold Plasma Prescription
Video instructions for using Mirari Cold Plasma Device – Y02 Pain in testis/scrotum (ICD-10:N50.9)
| Mild | Moderate | Severe |
| Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 1 (Infection) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 2 (Wound Healing) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 3 (Antiviral Therapy) Location: 0 (Localized) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 3 (Antiviral Therapy) Location: 0 (Localized) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 15 minutes, Evening: 15 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
Mode setting: 7 (Immunotherapy) Location: 1 (Sacrum) Morning: 30 minutes, Lunch: 30 minutes, Evening: 30 minutes |
| Total Morning: 60 minutes approx. $10 USD, Evening: 60 minutes approx. $10 USD |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
Total Morning: 120 minutes approx. $20 USD, Lunch: 120 minutes approx. $20 USD, Evening: 120 minutes approx. $20 USD, |
| Usual treatment for 7-60 days approx. $140 USD – $1200 USD | Usual treatment for 6-8 weeks approx. $2,520 USD – $3,360 USD |
Usual treatment for 3-6 months approx. $5,400 USD – $10,800 USD
|
 |
|
Use the Mirari Cold Plasma device to treat Pain in testis/scrotum effectively.
WARNING: MIRARI COLD PLASMA IS DESIGNED FOR THE HUMAN BODY WITHOUT ANY ARTIFICIAL OR THIRD PARTY PRODUCTS. USE OF OTHER PRODUCTS IN COMBINATION WITH MIRARI COLD PLASMA MAY CAUSE UNPREDICTABLE EFFECTS, HARM OR INJURY. PLEASE CONSULT A MEDICAL PROFESSIONAL BEFORE COMBINING ANY OTHER PRODUCTS WITH USE OF MIRARI.
Step 1: Cleanse the Skin
- Start by cleaning the affected area of the skin with a gentle cleanser or mild soap and water. Gently pat the area dry with a clean towel.
Step 2: Prepare the Mirari Cold Plasma device
- Ensure that the Mirari Cold Plasma device is fully charged or has fresh batteries as per the manufacturer’s instructions. Make sure the device is clean and in good working condition.
- Switch on the Mirari device using the power button or by following the specific instructions provided with the device.
- Some Mirari devices may have adjustable settings for intensity or treatment duration. Follow the manufacturer’s instructions to select the appropriate settings based on your needs and the recommended guidelines.
Step 3: Apply the Device
- Place the Mirari device in direct contact with the affected area of the skin. Gently glide or hold the device over the skin surface, ensuring even coverage of the area experiencing.
- Slowly move the Mirari device in a circular motion or follow a specific pattern as indicated in the user manual. This helps ensure thorough treatment coverage.
Step 4: Monitor and Assess:
- Keep track of your progress and evaluate the effectiveness of the Mirari device in managing your Pain in testis/scrotum. If you have any concerns or notice any adverse reactions, consult with your health care professional.
Note
This guide is for informational purposes only and should not replace the advice of a medical professional. Always consult with your healthcare provider or a qualified medical professional for personal advice, diagnosis, or treatment. Do not solely rely on the information presented here for decisions about your health. Use of this information is at your own risk. The authors of this guide, nor any associated entities or platforms, are not responsible for any potential adverse effects or outcomes based on the content.
Mirari Cold Plasma System Disclaimer
- Purpose: The Mirari Cold Plasma System is a Class 2 medical device designed for use by trained healthcare professionals. It is registered for use in Thailand and Vietnam. It is not intended for use outside of these locations.
- Informational Use: The content and information provided with the device are for educational and informational purposes only. They are not a substitute for professional medical advice or care.
- Variable Outcomes: While the device is approved for specific uses, individual outcomes can differ. We do not assert or guarantee specific medical outcomes.
- Consultation: Prior to utilizing the device or making decisions based on its content, it is essential to consult with a Certified Mirari Tele-Therapist and your medical healthcare provider regarding specific protocols.
- Liability: By using this device, users are acknowledging and accepting all potential risks. Neither the manufacturer nor the distributor will be held accountable for any adverse reactions, injuries, or damages stemming from its use.
- Geographical Availability: This device has received approval for designated purposes by the Thai and Vietnam FDA. As of now, outside of Thailand and Vietnam, the Mirari Cold Plasma System is not available for purchase or use.
References
- Gordhan CG, Sadeghi-Nejad H. Scrotal pain: evaluation and management. Korean J Urol. 2015;56(1):3-11.
- Davis JE, Silverman M. Scrotal emergencies. Emerg Med Clin North Am. 2011;29(3):469-484.
- Sharp VJ, Kieran K, Arlen AM. Testicular torsion: diagnosis, evaluation, and management. Am Fam Physician. 2013;88(12):835-840.
- Tracy CR, Steers WD, Costabile R. Diagnosis and management of epididymitis. Urol Clin North Am. 2008;35(1):101-108.
- Trojian TH, Lishnak TS, Heiman D. Epididymitis and orchitis: an overview. Am Fam Physician. 2009;79(7):583-587.
- Wang A, Stormont I, Siddiqui MM. A review of imaging modalities used in the diagnosis and management of scrotal trauma. Curr Urol Rep. 2017;18(12):98.
- HerniaSurge Group. International guidelines for groin hernia management. Hernia. 2018;22(1):1-165.
- Alsaikhan B, Alrabeeah K, Delouya G, Zini A. Epidemiology of varicocele. Asian J Androl. 2016;18(2):179-181.
- Baird DC, Meyers GJ, Hu JS. Testicular Cancer: Diagnosis and Treatment. Am Fam Physician. 2018;97(4):261-268.
- Scales CD Jr, Smith AC, Hanley JM, Saigal CS; Urologic Diseases in America Project. Prevalence of kidney stones in the United States. Eur Urol. 2012;62(1):160-165.
Related articles
Made in USA