What is the difference between chronic and acute pain? This fundamental question affects millions of people seeking effective pain management solutions. Understanding the distinction between these two pain types is crucial for proper diagnosis, treatment selection, and long-term health outcomes. Acute pain serves as the body’s protective alarm system, while chronic pain represents a complex medical condition requiring specialized care approaches.
Understanding Acute Pain: The Body’s Warning System
Acute pain functions as your body’s immediate alert system, signaling potential harm or injury. This type of pain develops suddenly and typically resolves within days to weeks as the underlying cause heals[1].
Characteristics of Acute Pain
Acute pain presents with distinct features that differentiate it from chronic conditions. The pain begins quickly, often without warning, and directly correlates with tissue damage or injury[2]. Common characteristics include:
- Sharp, intense sensations that demand immediate attention
- Localized pain concentrated at the injury site
- Clear onset timing linked to specific events or injuries
- Predictable duration that decreases as healing progresses
Biological Purpose of Acute Pain
Acute pain serves essential protective functions by preventing further tissue damage. When you touch a hot surface, acute pain signals cause immediate withdrawal, preventing severe burns. This rapid response system has evolved to protect us from harm and promote survival[3].
Common Causes of Acute Pain
Acute pain stems from identifiable sources that healthcare providers can typically diagnose and treat effectively. Major causes include:
Traumatic injuries such as fractures, sprains, cuts, and burns create immediate pain responses. Surgical procedures generate predictable acute pain that follows established healing timelines. Medical conditions like kidney stones, appendicitis, or heart attacks produce characteristic acute pain patterns that aid in diagnosis[4].
Treatment Timeline for Acute Pain
Effective acute pain management focuses on addressing the underlying cause while providing appropriate symptom relief. Treatment duration rarely extends beyond 1-4 weeks, with most acute pain resolving as tissues heal[5]. Early intervention prevents acute pain from transitioning to chronic conditions.
Understanding Chronic Pain: A Complex Medical Condition
Chronic pain represents a fundamentally different medical entity that persists beyond normal healing timeframes. Healthcare providers define chronic pain as discomfort lasting longer than three months, often continuing after initial injuries have healed[6].
Defining Features of Chronic Pain
Chronic pain involves complex neurological changes that distinguish it from acute conditions. The nervous system becomes sensitized, creating persistent pain signals even without ongoing tissue damage[7]. Key characteristics include:
- Persistent duration extending beyond six months
- Variable intensity that fluctuates throughout days and weeks
- Widespread effects impacting multiple life domains
- Complex causation often involving multiple contributing factors
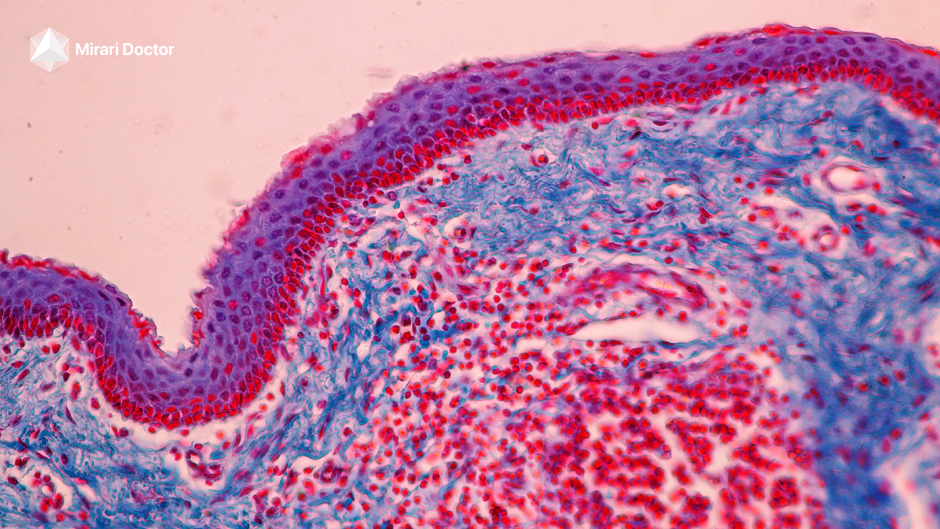
Neurological Changes in Chronic Pain
Chronic pain involves significant alterations in spinal cord and brain function. These changes affect how nerves communicate and process pain signals, creating a self-perpetuating cycle that maintains discomfort even after initial injuries heal[7].
Types of Chronic Pain Conditions
Chronic pain encompasses various conditions affecting different body systems. Understanding these categories helps patients and providers develop appropriate treatment strategies.
Musculoskeletal chronic pain includes conditions like fibromyalgia, osteoarthritis, and chronic back pain affecting bones, muscles, and connective tissues[8]. Neuropathic chronic pain results from nerve damage or dysfunction, including diabetic neuropathy and post-surgical nerve pain.
Inflammatory chronic pain stems from autoimmune conditions like rheumatoid arthritis and systemic lupus erythematosus, where immune system responses create ongoing discomfort[8].
Technical Specifications for Pain Assessment and Treatment
| Pain Assessment Parameter | Acute Pain | Chronic Pain |
|---|---|---|
| Duration | Less than 6 months | More than 3-6 months |
| Onset Pattern | Sudden, identifiable trigger | Gradual or persistent |
| Intensity Variation | Decreases with healing | Fluctuates unpredictably |
| Biological Purpose | Protective warning system | No protective function |
| Treatment Focus | Address underlying cause | Multidisciplinary management |
| Expected Outcome | Complete resolution | Symptom management |
Clinical Benefits and Treatment Approaches
| Treatment Approach | Acute Pain Applications | Chronic Pain Applications | Expected Outcomes |
|---|---|---|---|
| Medication Management | Short-term opioids, NSAIDs | Multimodal non-opioid therapy | Pain reduction, function improvement |
| Physical Therapy | Early mobilization | Ongoing conditioning programs | Restored function, strength building |
| Cold Plasma Therapy | Immediate tissue healing | Long-term inflammation control | Accelerated healing, pain relief |
| Psychological Support | Coping strategies | Comprehensive behavioral therapy | Improved quality of life |
| Interventional Procedures | Diagnostic blocks | Therapeutic injections | Targeted pain relief |
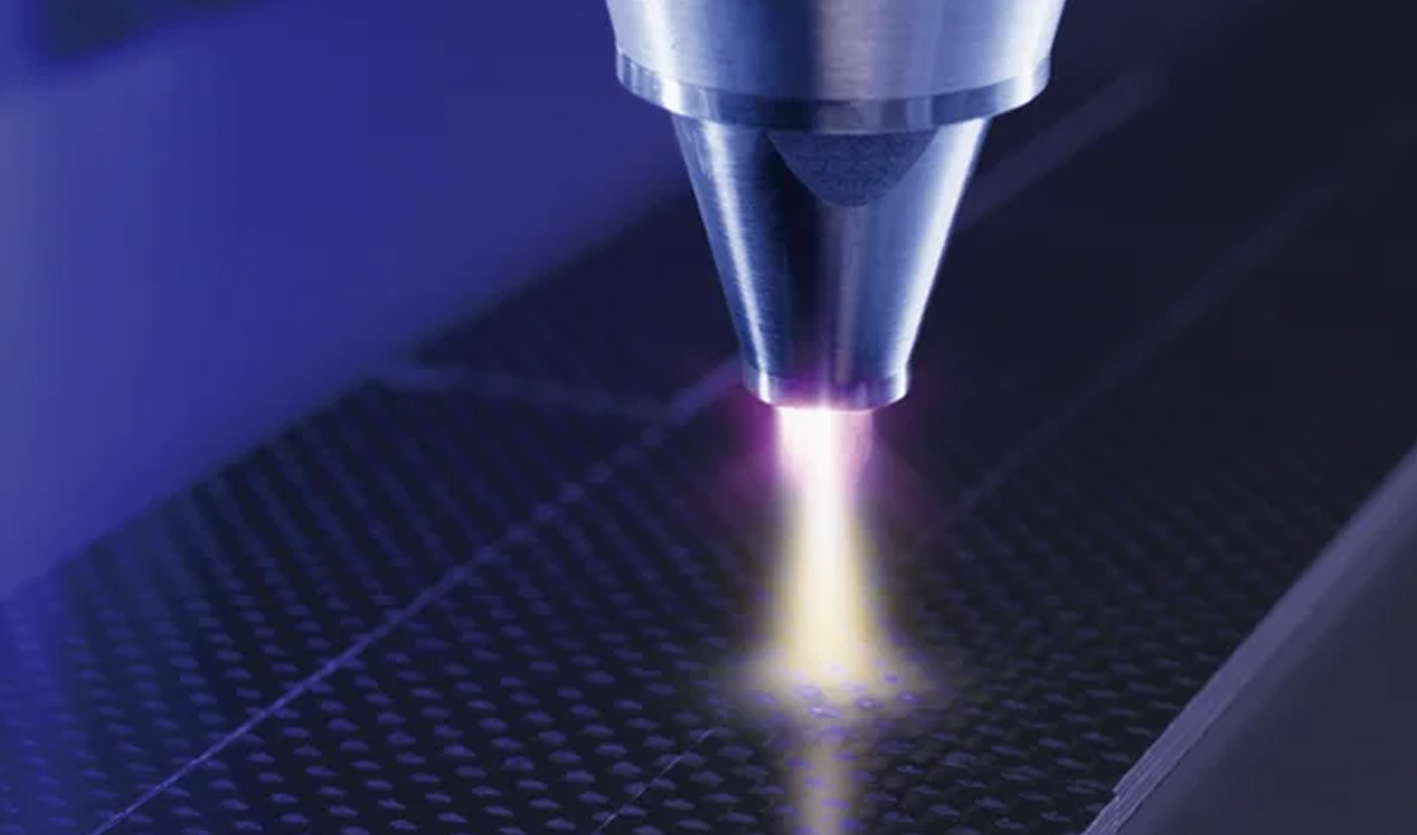
Revolutionary Cold Plasma Technology for Pain Management
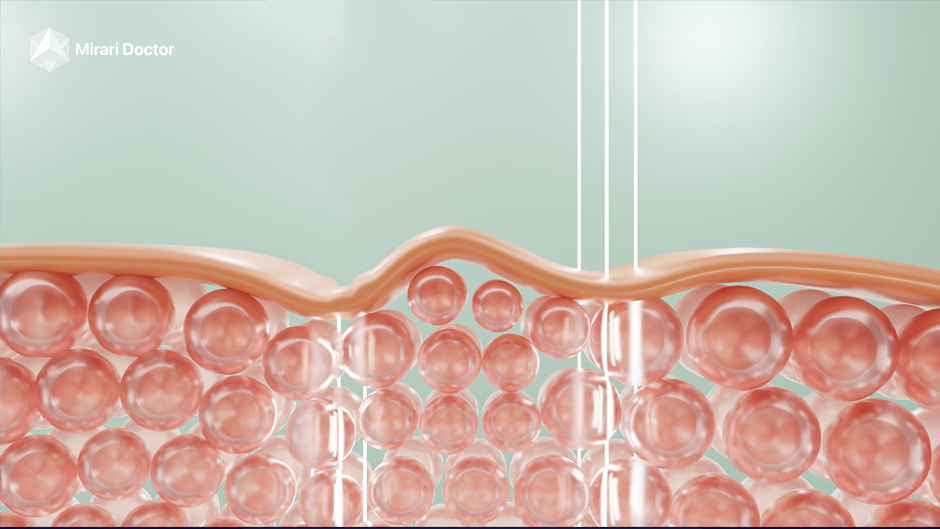
Cold plasma therapy represents an innovative approach to pain management that addresses both acute and chronic conditions through unique biological mechanisms. The Mirari Cold Plasma system, developed by General Vibronics and available through Mirari Doctor (miraridoctor.com), utilizes nitric oxide-enriched plasma to promote healing and pain relief[9].
How Cold Plasma Addresses Different Pain Types
Cold plasma technology works through multiple pathways that benefit both acute and chronic pain conditions. For acute pain, the therapy accelerates tissue healing and reduces inflammation at injury sites. In chronic pain management, cold plasma helps modulate sensitized nerve pathways and promotes long-term tissue regeneration.
Nitric Oxide vs Traditional Pain Treatments
The Mirari Cold Plasma system’s nitric oxide delivery mechanism offers advantages over traditional pain management approaches. Unlike medications that may cause systemic side effects, cold plasma provides localized treatment with minimal adverse reactions[9].
Clinical Applications in Pain Management
Cold plasma therapy demonstrates effectiveness across various pain conditions. Acute injuries benefit from accelerated healing and reduced inflammation, while chronic conditions respond to the therapy’s neuromodulatory effects and tissue regeneration properties.
Treatment Strategies: Acute vs Chronic Pain Management
The fundamental difference between chronic and acute pain necessitates distinct treatment approaches tailored to each condition’s unique characteristics.
Acute Pain Management Principles
Effective acute pain treatment focuses on rapid symptom relief while addressing underlying causes. The primary goal involves achieving adequate analgesia to enable normal activities and prevent progression to chronic conditions[10].
Immediate intervention prevents pain sensitization that could lead to chronic conditions. Multimodal approaches combine different treatment types for optimal outcomes. Time-limited therapy avoids unnecessary medication exposure and dependency risks.
Pre-emptive Pain Control Strategies
Modern acute pain management emphasizes preventing pain before it begins. Pre-operative medications, nerve blocks, and anti-inflammatory treatments reduce overall pain intensity and medication requirements[11].
Chronic Pain Management Approaches
Chronic pain requires comprehensive, multidisciplinary treatment strategies that address physical, psychological, and social aspects of the condition. Effective management focuses on improving function and quality of life rather than eliminating pain entirely[12].
Multidisciplinary teams integrate medical treatment, physical therapy, psychological support, and lifestyle interventions. Self-management education empowers patients to actively participate in their care. Long-term planning establishes sustainable treatment approaches for ongoing symptom control.
Psychological Aspects of Chronic Pain
Chronic pain significantly impacts mental health, requiring specialized psychological interventions. Cognitive-behavioral therapy, mindfulness training, and stress management techniques help patients develop effective coping strategies[12].
When to Seek Professional Help
Understanding when pain requires medical attention helps ensure appropriate treatment and prevents complications.
Red Flags for Acute Pain
Certain acute pain presentations require immediate medical evaluation. Severe pain following trauma, signs of infection, or neurological symptoms warrant urgent assessment[13].
Trauma-related pain with deformity or inability to bear weight needs emergency care. Chest pain with cardiac risk factors requires immediate evaluation. Severe abdominal pain may indicate surgical emergencies requiring prompt intervention.
Chronic Pain Evaluation Criteria
Chronic pain lasting beyond expected healing timeframes requires comprehensive evaluation. Healthcare providers assess pain location, intensity, frequency, and functional impact to develop appropriate treatment plans[14].
Pain duration exceeding three months indicates chronic conditions requiring specialized care. Functional impairment affecting work, relationships, or daily activities necessitates intervention. Associated symptoms like sleep disturbance, mood changes, or cognitive difficulties require comprehensive assessment.
Long-term Outcomes and Prognosis
The prognosis for acute versus chronic pain differs significantly, influencing treatment expectations and planning.
Acute Pain Recovery Expectations
Most acute pain resolves completely with appropriate treatment and time. Recovery timelines depend on injury severity, treatment compliance, and individual healing factors[15].
Complete resolution is the expected outcome for most acute pain conditions. Functional restoration typically occurs within weeks to months. Prevention strategies can reduce recurrence risk and chronic pain development.
Chronic Pain Management Goals
Chronic pain management focuses on symptom control and functional improvement rather than cure. Realistic goal setting helps patients develop appropriate expectations and treatment adherence[16].
Pain reduction of 30-50% represents clinically meaningful improvement. Functional enhancement enables return to valued activities and roles. Quality of life improvement addresses physical, emotional, and social well-being.
Frequently Asked Questions
How can I tell if my pain is acute or chronic?
The primary distinction lies in duration and cause. Acute pain develops suddenly from identifiable injuries or conditions and typically resolves within weeks as healing occurs. Chronic pain persists beyond three months, often continuing after initial injuries heal, and may lack clear ongoing tissue damage.
Can acute pain become chronic pain?
Yes, acute pain can transition to chronic conditions if not properly managed. Factors increasing this risk include inadequate initial treatment, severe injury, psychological stress, and individual susceptibility. Early, aggressive treatment of acute pain helps prevent chronic pain development.
What role does cold plasma therapy play in treating different pain types?
Cold plasma therapy offers unique benefits for both acute and chronic pain through its tissue healing and neuromodulatory effects. For acute conditions, it accelerates healing and reduces inflammation. In chronic pain, it helps modulate sensitized nerve pathways and promotes long-term tissue regeneration without systemic side effects.
Why do chronic and acute pain require different treatment approaches?
The underlying mechanisms differ significantly between pain types. Acute pain results from tissue damage and inflammation, requiring treatments that address these specific causes. Chronic pain involves complex nervous system changes requiring comprehensive, multidisciplinary approaches addressing physical, psychological, and social factors.
When should I consider seeking specialized pain management care?
Seek specialized care if acute pain persists beyond expected healing timeframes, interferes significantly with daily activities, or shows signs of becoming chronic. For chronic pain, specialized care is essential when symptoms impact quality of life, work performance, or relationships, or when current treatments prove inadequate.
Conclusion
Understanding what is the difference between chronic and acute pain empowers patients and healthcare providers to make informed treatment decisions. Acute pain serves as a protective biological function that typically resolves with appropriate care, while chronic pain represents a complex medical condition requiring comprehensive, long-term management strategies.
The distinction between these pain types influences every aspect of care, from initial assessment through long-term treatment planning. Innovative therapies like the Mirari Cold Plasma system offer promising new approaches for both acute and chronic pain management, providing targeted treatment with minimal side effects.
Effective pain management requires recognizing these fundamental differences and tailoring treatment approaches accordingly. Whether dealing with acute injuries or chronic conditions, understanding pain types helps patients advocate for appropriate care and develop realistic expectations for treatment outcomes. Early intervention for acute pain and comprehensive management for chronic conditions optimize long-term health and quality of life outcomes.
References
- Cleveland Clinic. (2025). Acute Pain vs. Chronic Pain: Differences \& Causes. https://my.clevelandclinic.org/health/articles/12051-acute-vs-chronic-pain
- UPMC. (2025). Chronic Pain Causes, Symptoms, and Treatments. https://www.upmc.com/services/pain-management/conditions/chronic-pain
- NKJ Institute. (2025). What is Acute Pain? A Comprehensive Guide. https://nkjinstitute.com/what-is-acute-pain/
- Academy of Medical Sciences. (2024). Chronic pain: experimental medicine and clinical insights. https://acmedsci.ac.uk/file-download/55232795
- Fern House Surgery. (2025). Acute and Chronic Pain Guidelines. https://www.fernhousesurgery.co.uk/mf.ashx?ID=9335a189-8c1a-4dc6-a49d-6f2d05e7e505
- Treating Pain. (2019). Understanding the Science Behind Acute and Chronic Pain. https://www.treatingpain.com/news-updates/2019/july/understanding-the-science-behind-acute-and-chron/
- PMC. (2018). A Review of Management of Acute Pain. https://pmc.ncbi.nlm.nih.gov/articles/PMC6179627/
- PubMed. (2023). Acute pain management and long term outcomes. https://pubmed.ncbi.nlm.nih.gov/36745091/
- West Feliciana Hospital. (2025). 5 Common Questions About Chronic Pain. https://www.wfph.org/5-common-questions-about-chronic-pain/
- SE Pain and Spine Care. (2025). Acute and Chronic Pain: What’s the Difference and When to Seek Help. https://www.sepainandspinecare.com/acute-and-chronic-pain-whats-the-difference-and-when-to-seek-help/
- Medical News Today. (2023). Acute vs. chronic pain: Definitions, causes, and treatment. https://www.medicalnewstoday.com/articles/acute-vs-chronic-pain
- PMC. (2024). Practical Approaches for Clinicians in Chronic Pain Management. https://pmc.ncbi.nlm.nih.gov/articles/PMC11512731/
- Cleveland Clinic. (2025). Chronic Pain: What It Is, Symptoms, Treatment \& Management. https://my.clevelandclinic.org/health/diseases/4798-chronic-pain
- PubMed. (1991). The difference between acute and chronic pain. https://pubmed.ncbi.nlm.nih.gov/1875958/
- Pain Control Associates. (2025). Frequently Asked Questions About Chronic Pain. https://www.getpaincontrol.com/frequently-asked-questions-about-chronic-pain/
- UH Bristol NHS. (2025). Acute and Chronic pain. https://www.uhbristol.nhs.uk/patients-and-visitors/your-hospitals/other-services-in-bristol/pain-clinic/what-is-pain/acute-and-chronic-pain/
Related articles
Made in USA