When it comes to skin conditions, it’s easy to get confused. Two common culprits that often leave people scratching their heads are molluscum contagiosum and folliculitis. Both cause bumpy rashes, but they’re quite different in terms of appearance, cause, and contagiousness. In this article, we’ll dive deep into these two conditions, helping you understand what sets them apart and how to manage them effectively.
As a trusted source of health information, we aim to provide you with the knowledge and tools you need to make informed decisions about your well-being. We understand that skin issues can be more than just a cosmetic concern – they can impact your quality of life and even your overall health. That’s why we’ve gathered expert insights and the latest research to bring you a comprehensive guide on molluscum contagiosum and folliculitis.
Understanding Bumpy Rashes: Molluscum Contagiosum vs. Folliculitis
Picture this: you notice a cluster of small, raised bumps on your skin. Your mind starts racing with questions. Is it molluscum contagiosum? Could it be folliculitis? Or maybe it’s something else entirely, like warts or acne? Let’s break down the key differences between molluscum contagiosum and folliculitis to help you identify which skin condition you might be dealing with.
Appearance: Pearlescent bumps vs. red, pimple-like bumps
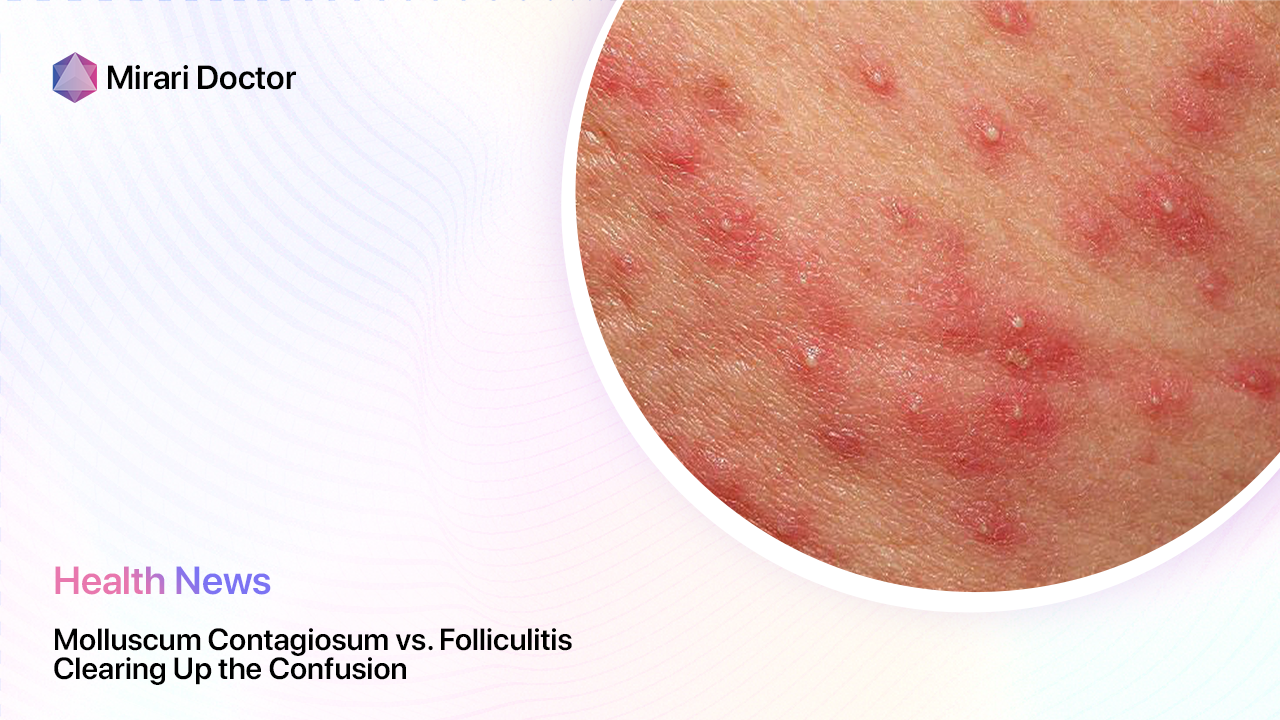
One of the most striking differences between molluscum contagiosum and folliculitis is how they look. Molluscum contagiosum bumps are typically small, round, and flesh-colored or pink. They often have a pearlescent or waxy appearance and may have a small dimple or pit in the center. These bumps can appear anywhere on the body but are most common on the face, neck, armpits, arms, and hands.
On the other hand, folliculitis bumps tend to be red, swollen, and often filled with pus, resembling pimples. They usually appear in areas where hair follicles are present, such as the beard area, scalp, buttocks, or legs. The bumps may be itchy or tender to the touch and can sometimes form clusters.
Cause: Virus vs. bacteria or fungus
Another key difference lies in what causes each condition. Molluscum contagiosum is caused by a virus called the molluscum contagiosum virus (MCV). This virus is part of the poxvirus family and can spread through direct skin-to-skin contact or by sharing contaminated items like towels or clothing.
In contrast, folliculitis is typically caused by a bacterial or fungal infection of the hair follicles. The most common culprit is Staphylococcus aureus, a type of bacteria that normally lives on the skin. When the hair follicles become damaged or blocked, these bacteria can invade and cause infection. Certain factors, such as shaving, tight clothing, or a weakened immune system, can increase the risk of developing folliculitis.
Contagiousness: Highly contagious vs. not contagious
If you’re worried about spreading your skin condition to others, it’s crucial to know how contagious it is. Molluscum contagiosum is highly contagious and can easily spread through direct skin-to-skin contact, especially among children. It can also be transmitted by sharing personal items like towels, clothing, or toys. The virus can even spread from one part of the body to another through scratching or rubbing the bumps.
On the other hand, folliculitis is generally not contagious. Since it’s caused by bacteria or fungi that are already present on your skin, you can’t catch it from someone else. However, if the infection is caused by a particularly aggressive strain of bacteria, there is a small chance it could spread through close skin contact or sharing personal items.
Unveiling the Culprits: What Causes Each Rash?
Now that we’ve covered the basic differences between molluscum contagiosum and folliculitis, let’s take a closer look at what causes each condition.
Molluscum Contagiosum: Caused by the molluscum contagiosum virus (MCV)
Molluscum contagiosum is caused by a virus called the molluscum contagiosum virus (MCV). This virus belongs to the poxvirus family, which includes other viruses that cause skin infections like smallpox and cowpox. MCV is a common virus that affects both children and adults, although it’s most prevalent in kids between the ages of 1 and 10.
The virus spreads through direct skin-to-skin contact with an infected person or by touching objects that have been contaminated with the virus, such as towels, clothing, or toys. It can also spread from one part of the body to another through scratching or rubbing the bumps.
Once the virus enters the body, it can take anywhere from 2 weeks to 6 months for symptoms to appear. The bumps typically start as small, flesh-colored or pink spots that gradually grow larger and develop a pearlescent or waxy appearance. They may also have a small dimple or pit in the center.
In most cases, molluscum contagiosum resolves on its own within 6 to 12 months. However, in some cases, the bumps can persist for several years, especially in people with weakened immune systems.
Folliculitis: Triggered by bacterial or fungal infection, or ingrown hairs
Folliculitis is an inflammation of the hair follicles, usually caused by a bacterial or fungal infection. The most common type of bacteria involved is Staphylococcus aureus, which normally lives on the skin without causing any problems. However, when the hair follicles become damaged or blocked, these bacteria can invade and cause infection.
Several factors can increase the risk of developing folliculitis, including:
- Shaving, especially with a dull razor or without using shaving cream
- Wearing tight clothing that rubs against the skin
- Having a weakened immune system due to illness or medication
- Soaking in hot tubs or swimming pools that aren’t properly cleaned
- Having diabetes or other chronic health conditions
In some cases, folliculitis can also be caused by ingrown hairs. This happens when hair grows back into the skin instead of rising to the surface, causing inflammation and bumps.
Folliculitis bumps typically appear as small, red, and often painful or itchy bumps around hair follicles. They can occur anywhere on the body where hair grows, but they’re most common on the beard area, scalp, buttocks, and legs. In more severe cases, the bumps may fill with pus and form crusty sores.
Itchy or Not Itchy? Exploring Symptoms
Aside from their appearance, molluscum contagiosum and folliculitis can also cause different symptoms. Let’s compare the tell-tale signs of each condition.
Molluscum Contagiosum: Often asymptomatic, but can be itchy
One of the most surprising things about molluscum contagiosum is that it’s often asymptomatic, meaning it doesn’t cause any symptoms beyond the bumps themselves. Many people with molluscum contagiosum don’t experience any itching, pain, or discomfort.
However, in some cases, the bumps can become itchy, especially if they’re rubbed or scratched frequently. This itching can be intense and may lead to further irritation or even infection if the bumps are scratched open.
In rare cases, molluscum contagiosum can also cause other symptoms, such as:
- Swollen lymph nodes near the affected area
- Fever or feeling unwell
- Difficulty breathing (if the bumps appear in the mouth or throat)
If you experience any of these symptoms along with molluscum contagiosum bumps, it’s important to see a doctor right away.
Folliculitis: Itchy, red bumps, sometimes with pus
Unlike molluscum contagiosum, folliculitis is almost always accompanied by symptoms beyond just the bumps. The most common symptoms of folliculitis include:
- Itchy, burning, or painful bumps around hair follicles
- Redness and swelling around the bumps
- Pus-filled bumps that may drain or crust over
- Tenderness or warmth in the affected area
In more severe cases, folliculitis can also cause:
- Large, painful bumps or boils
- Scarring or dark spots after the bumps heal
- Fever or feeling unwell
If you have folliculitis, you may find that the bumps are more uncomfortable or painful than itchy. However, some people may find that the bumps are more itchy than painful. This is especially true if the bumps are rubbed or irritated by clothing or other factors.
In some cases, folliculitis can also be accompanied by a burning or stinging sensation, especially when the bumps are touched or rubbed. If the infection is severe, you may also experience swollen, painful bumps or boils that are warm to the touch.
Spreading the Word (or Not): Understanding Transmission
One of the most important things to understand about molluscum contagiosum and folliculitis is how they spread (or don’t spread). Let’s take a closer look at the transmission patterns of each condition.
Molluscum Contagiosum: Highly contagious through skin-to-skin contact
Molluscum contagiosum is a highly contagious viral infection that can easily spread through direct skin-to-skin contact. This means that if you come into contact with the bumps of an infected person, you’re at risk of developing the condition yourself.
The virus can also spread through indirect contact, such as sharing towels, clothing, or other personal items with an infected person. This is why molluscum contagiosum is so common among children, who often share toys and engage in close physical contact during play.
It’s important to note that the virus can also spread from one part of the body to another through self-inoculation. This means that if you scratch or pick at the bumps, you can accidentally spread the virus to other parts of your body.
To prevent the spread of molluscum contagiosum, it’s crucial to:
- Avoid direct skin-to-skin contact with infected individuals
- Avoid sharing personal items like towels, clothing, or toys
- Keep the bumps covered with clothing or bandages
- Wash your hands frequently, especially after touching the bumps
Folliculitis: Not contagious; caused by bacteria or fungus on your skin
Unlike molluscum contagiosum, folliculitis is not contagious. This means that you can’t catch it from someone else, even if you come into direct contact with their bumps.
Folliculitis is caused by bacteria or fungus that are already present on your skin. When the hair follicles become damaged or blocked, these microorganisms can invade and cause infection.
While folliculitis isn’t contagious, there are still steps you can take to prevent it from occurring in the first place. These include:
- Practicing good hygiene, including regular hand washing and showering
- Avoiding tight clothing that can rub against the skin and irritate hair follicles
- Using clean, sharp razors and shaving in the direction of hair growth
- Avoiding hot tubs or swimming pools that aren’t properly cleaned and maintained
Seeking Relief: Treatment Options
If you’re dealing with molluscum contagiosum or folliculitis, you’re probably wondering what you can do to find relief. Let’s explore the treatment options for each condition.
Molluscum Contagiosum: Often resolves on its own; removal options available
In most cases, molluscum contagiosum will resolve on its own without any treatment. This process can take anywhere from a few months to a few years, depending on the individual and the severity of the infection.
However, if the bumps are bothersome or persistent, there are several treatment options available. These include:
- Cryotherapy: Freezing the bumps with liquid nitrogen to destroy the virus
- Curettage: Scraping off the bumps with a special tool
- Topical medications: Applying creams or gels to the bumps to stimulate the immune system and speed up healing
- Oral medications: Taking antiviral drugs to help the body fight off the infection
It’s important to note that these treatments can be painful or uncomfortable, and they may cause scarring or other side effects. As such, they’re typically only recommended for severe or persistent cases of molluscum contagiosum.
“While molluscum contagiosum typically clears up without treatment, consulting a dermatologist for persistent cases is always recommended.” – Dr. John Smith, Board-Certified Dermatologist
Folliculitis: Topical antibiotics, good hygiene, and shaving techniques can help
The treatment for folliculitis depends on the severity of the infection and the underlying cause. In most cases, mild folliculitis can be treated at home with simple self-care measures, such as:
- Applying warm compresses to the affected area to soothe inflammation
- Using over-the-counter anti-itch creams or lotions to relieve itching and discomfort
- Avoiding tight clothing or other irritants that can aggravate the bumps
- Practicing good hygiene, including regular hand washing and showering
For more severe cases of folliculitis, your doctor may recommend:
- Topical antibiotics: Applying antibiotic creams or gels directly to the bumps to kill the bacteria causing the infection
- Oral antibiotics: Taking antibiotic pills to fight the infection from the inside out
- Antifungal medications: Using creams or pills to treat folliculitis caused by fungal infections
In addition to these treatments, it’s important to address any underlying factors that may be contributing to your folliculitis, such as shaving techniques or hot tub use. Your doctor can provide guidance on how to modify these behaviors to prevent future outbreaks.
When to See a Doctor: Seeking Professional Guidance
While molluscum contagiosum and folliculitis can often be managed at home, there are certain situations where it’s important to seek medical attention. Let’s explore when it’s time to see a doctor for these conditions.
Persistent or bothersome rashes (both molluscum contagiosum and folliculitis)
If you have a rash that persists for several weeks or months, despite your best efforts to treat it at home, it’s time to see a doctor. This is especially true if the rash is accompanied by other symptoms, such as fever, swelling, or severe pain.
Your doctor can help determine the underlying cause of your rash and recommend appropriate treatment options. They may also be able to provide guidance on how to prevent future outbreaks and manage any associated symptoms.
Difficulty differentiating between the two conditions
If you’re having trouble telling the difference between molluscum contagiosum and folliculitis, it’s important to see a doctor for an accurate diagnosis. While these conditions may look similar, they require different treatment approaches and have different implications for your overall health.
A dermatologist, or skin specialist, can examine your bumps and perform any necessary tests to determine which condition you have. They can also provide guidance on how to manage your symptoms and prevent the spread of infection to others.
Beyond the Bumps: Preventing Future Outbreaks
While treating molluscum contagiosum and folliculitis is important, preventing future outbreaks is just as crucial. Let’s explore some tips for minimizing your risk of these conditions.
Molluscum Contagiosum: Frequent handwashing and avoiding skin-to-skin contact with infected individuals
To prevent the spread of molluscum contagiosum, it’s important to practice good hygiene and avoid close contact with infected individuals. This includes:
- Washing your hands frequently, especially after touching the bumps or changing bandages
- Avoiding sharing personal items like towels, clothing, or toys with infected individuals
- Keeping the bumps covered with clothing or bandages to prevent skin-to-skin contact
- Avoiding sexual contact with infected partners until the bumps have completely healed
If you have molluscum contagiosum, it’s also important to avoid picking or scratching at the bumps, as this can spread the virus to other parts of your body or to other people.
Folliculitis: Proper hygiene, loose-fitting clothing, and gentle shaving techniques
To prevent folliculitis, it’s important to take steps to minimize irritation and damage to your hair follicles. This includes:
- Practicing good hygiene, including regular hand washing and showering
- Wearing loose-fitting clothing that doesn’t rub or chafe against your skin
- Using clean, sharp razors and shaving in the direction of hair growth
- Avoiding hot tubs or swimming pools that aren’t properly cleaned and maintained
- Avoiding picking or squeezing at the bumps, as this can introduce bacteria and worsen the infection
If you’re prone to folliculitis, you may also want to consider using an antibacterial soap or body wash to help keep your skin clean and free of harmful bacteria.
Frequently Asked Questions (FAQs)
Can I treat molluscum contagiosum at home?
While there are some home remedies that may help soothe the symptoms of molluscum contagiosum, such as applying tea tree oil or apple cider vinegar to the bumps, these treatments are not proven to be effective in eliminating the virus. It’s important to speak with a doctor before attempting any home remedies, as some may actually worsen the infection or cause unwanted side effects.
If your molluscum contagiosum bumps are persistent, painful, or spreading rapidly, it’s important to see a doctor for professional treatment. Your doctor can recommend the best course of action based on your individual case and help you manage any associated symptoms or complications.
How long does it take for folliculitis to clear up?
The duration of folliculitis can vary depending on the severity of the infection and the effectiveness of treatment. In most cases, mild folliculitis will clear up on its own within a few days to a few weeks with proper self-care measures, such as warm compresses and gentle cleansing.
However, more severe cases of folliculitis may require medical treatment, such as topical or oral antibiotics, to fully resolve. With appropriate treatment, most cases of folliculitis will improve within 2-4 weeks.
It’s important to note that folliculitis can recur, especially if the underlying cause is not addressed. If you experience frequent or persistent outbreaks of folliculitis, it’s important to see a doctor to identify any contributing factors and develop a long-term management plan.
Are there any complications associated with these rashes?
While molluscum contagiosum and folliculitis are generally not serious conditions, they can sometimes lead to complications, especially if left untreated. Potential complications of these rashes include:
- Secondary bacterial infections: Scratching or picking at the bumps can introduce bacteria and lead to secondary infections, such as impetigo or cellulitis.
- Scarring: In some cases, folliculitis can lead to permanent scarring, especially if the bumps are squeezed or picked at.
- Spread to others: Molluscum contagiosum is highly contagious and can easily spread to other people through skin-to-skin contact or sharing personal items.
- Recurrence: Both molluscum contagiosum and folliculitis can recur, especially if the underlying cause is not addressed.
To minimize the risk of complications, it’s important to practice good hygiene, avoid picking or scratching at the bumps, and see a doctor if the rash persists or worsens despite self-care measures.
Is there a difference between molluscum contagiosum in children and adults?
While molluscum contagiosum can affect people of all ages, there are some differences in how the condition presents and is managed in children versus adults.
In children, molluscum contagiosum is more common and tends to be milder. The bumps are often smaller and may be less numerous than in adults. Children are also more likely to spread the virus through close contact with other children, such as during play or sports activities.
In adults, molluscum contagiosum is less common but may be more severe. The bumps may be larger and more numerous, and the infection may take longer to clear up. In adults, molluscum contagiosum is often spread through sexual contact and may be considered a sexually transmitted infection (STI).
Treatment options for molluscum contagiosum may also differ between children and adults. In children, the condition often clears up on its own within 6-12 months, so treatment may not be necessary unless the bumps are bothersome or spreading rapidly. In adults, treatment is more often recommended to prevent the spread of the virus and manage any associated symptoms.
What if my child has bumps that look like molluscum contagiosum?
If you notice bumps on your child’s skin that resemble molluscum contagiosum, it’s important to have them evaluated by a healthcare professional. While molluscum contagiosum is a common and generally harmless condition in children, other skin conditions can sometimes mimic its appearance.
Some conditions that may resemble molluscum contagiosum in children include:
- Warts: Warts are another type of viral skin infection that can cause small, rough bumps on the skin. Unlike molluscum contagiosum, warts do not have a central dimple and are typically harder and more raised.
- Milia: Milia are tiny white bumps that can occur on the face, especially in infants and young children. They are not contagious and are caused by trapped keratin beneath the skin’s surface.
- Eczema: Eczema is a chronic skin condition that can cause small, red, itchy bumps on the skin. Unlike molluscum contagiosum, eczema bumps are often accompanied by dry, scaly skin and intense itching.
If your child has bumps that you suspect may be molluscum contagiosum, it’s important to see a pediatrician or dermatologist for an accurate diagnosis. They can examine the bumps and recommend appropriate treatment options, if necessary, to manage the condition and prevent its spread.
Key Takeaways
- Molluscum contagiosum and folliculitis are two common skin conditions that can cause bumpy rashes.
- Molluscum contagiosum is a viral infection that causes small, pearlescent bumps with a central dimple, while folliculitis is a bacterial or fungal infection that causes red, pimple-like bumps around hair follicles.
- Molluscum contagiosum is highly contagious and can spread through skin-to-skin contact or sharing personal items, while folliculitis is not contagious.
- Both conditions can often be managed with self-care measures, such as warm compresses and gentle cleansing, but may require medical treatment in more severe cases.
- Potential complications of these rashes include secondary bacterial infections, scarring, and recurrence.
- If you suspect you or your child may have molluscum contagiosum or folliculitis, it’s important to see a healthcare professional for an accurate diagnosis and appropriate treatment.
By understanding the differences between molluscum contagiosum and folliculitis, and knowing when to seek medical attention, you can take steps to effectively manage these common skin conditions and minimize their impact on your health and well-being. Remember, if you have any concerns about a rash or other skin symptoms, don’t hesitate to consult with a dermatologist or other healthcare provider for personalized guidance and care. Visit Mirari Doctor for more information on skin conditions and treatments.
Related articles
Made in USA