Topical steroid withdrawal (TSW), also known as steroid cream withdrawal or topical corticosteroid withdrawal syndrome, is a rare but serious condition that can occur when someone stops using topical steroid medications after prolonged or inappropriate use[1]. It is characterized by a severe worsening or “rebound” of skin inflammation and irritation, often spreading to new areas of the body.
The most common and distressing symptoms of topical steroid withdrawal include[1][2]:
- Burning, stinging skin that feels like it’s on fire
- Intense itching that doesn’t respond to usual treatments
- Raw, weeping, oozing skin from scratching and irritation
- Dry, scaly, flaky skin that sheds excessively
- Small red bumps (pustules) that may be itchy or painful
- Swelling (edema), especially on the face and around the eyes
- Skin thinning and fragility, making skin more prone to injury
- “Elephant skin” thickening and wrinkling, especially in elbow and knee creases
These skin symptoms often appear within days to weeks of stopping the topical steroid and can be more severe than the original skin condition being treated. They may last for weeks to months, and in some cases, full recovery can take years[1].
In addition to the skin manifestations, people going through TSW often experience[1][2]:
- Difficulty sleeping due to pain and itch
- Anxiety and depression related to the physical discomfort and visible skin changes
- Fatigue and tiredness that makes daily activities challenging
- Chills and sweating, especially at night
- Headaches and general flu-like symptoms
The psychological impact of TSW cannot be overstated. Many people feel isolated, anxious, and depressed due to the dramatic changes in their appearance and inability to find relief. Support from family, friends, and the TSW community is crucial during this difficult time.
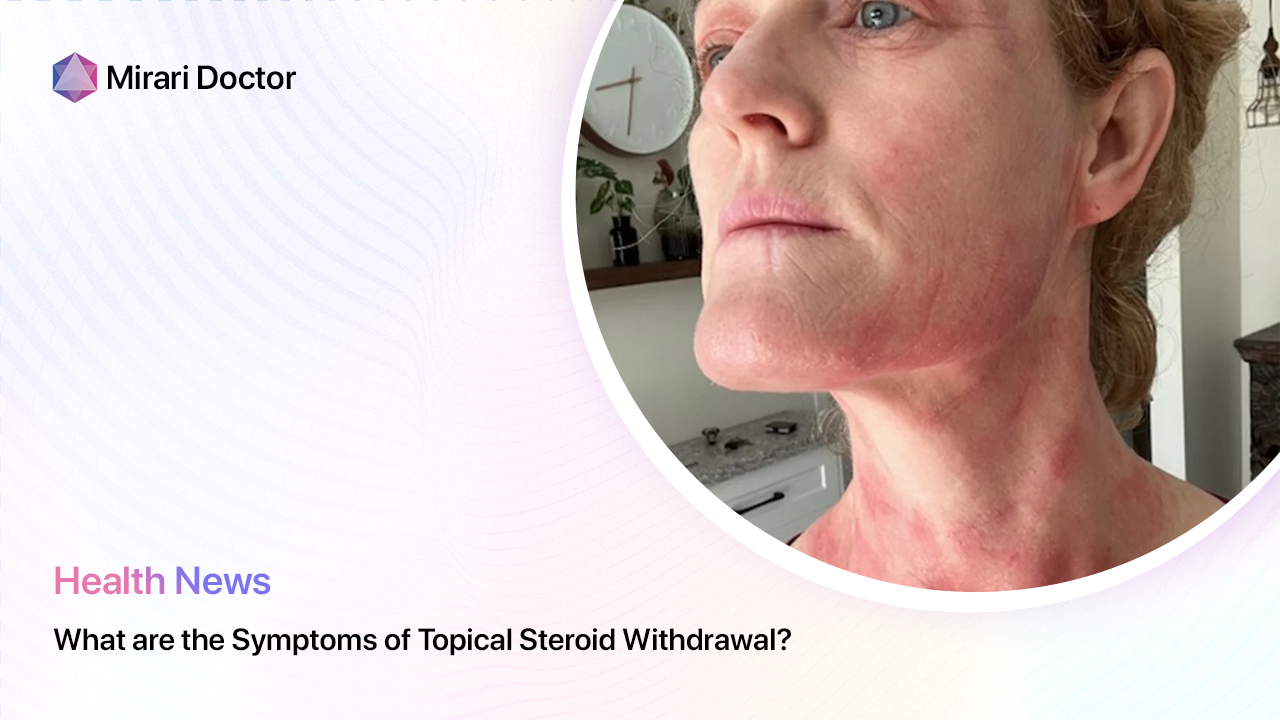
Skin Signs of Topical Steroid Withdrawal
While the symptoms of TSW can mimic a severe eczema flare, there are some characteristic skin signs that suggest steroid withdrawal[1]:
- Red sleeve sign – widespread redness (erythema) of the arms and legs
- Headlight sign – redness and swelling around the eyes with sparing of the nose (“headlight” pattern)
- Elephant wrinkles – thickened, wrinkled skin in areas like the elbows and knees
- Pustules – small, pus-filled bumps scattered on the skin
- Skin atrophy – thinning of the skin with increased visibility of blood vessels
- Hyperpigmentation – darkening of the skin in sun-exposed areas
The presence of these signs, along with a history of prolonged topical steroid use and onset of symptoms within weeks of stopping the medication, points to a diagnosis of TSW.
Variations in TSW Symptoms
It’s important to note that the specific symptoms and severity of TSW can vary from person to person. Factors that influence the presentation include[1][2]:
- Potency of the topical steroid – higher potency steroids are more likely to cause withdrawal
- Duration of use – longer use increases the risk and severity of TSW
- Frequency of application – applying steroids more than twice daily raises the chances of TSW
- Location of use – steroid withdrawal is more common on the face and genital area
- Age of the individual – children and older adults may be more susceptible to TSW
Some people may experience milder symptoms that resolve within a few weeks, while others have severe, debilitating symptoms that persist for months to years. It’s not entirely clear why some individuals develop TSW and others using similar amounts do not. More research is needed to understand the risk factors and mechanisms behind this condition.
Diagnosing Topical Steroid Withdrawal
There is no specific test or criteria for diagnosing TSW. Rather, doctors rely on a careful history and physical examination to determine if someone is experiencing steroid withdrawal[1].
Key factors that suggest TSW include:
- History of prolonged or frequent topical steroid use, especially on the face or genital area
- Worsening of skin symptoms within days to weeks of stopping the steroid
- Burning and stinging skin pain that is more pronounced than itching
- Redness and swelling that spreads beyond the original treatment area
- Failure to respond to usual eczema or psoriasis treatments
A skin biopsy can be helpful to rule out other conditions like psoriasis or fungal infections that may mimic TSW. However, the biopsy findings in TSW are often nonspecific and not diagnostic on their own.
It’s important for individuals who suspect they have TSW to see a dermatologist familiar with this condition. Many doctors are not aware of the potential for steroid withdrawal and may misdiagnose it as an eczema flare or psoriasis. A knowledgeable dermatologist can help guide the appropriate diagnosis and management.
Ruling Out Other Conditions
Several skin conditions can present with symptoms similar to TSW and need to be ruled out. These include:
- Atopic dermatitis (eczema) – may have intense itch and redness, but not usually burning/stinging pain; responds to topical steroids[2]
- Psoriasis – well-defined, thick, scaly plaques; may improve with topical steroids[3]
- Contact dermatitis – red, blistering rash from exposure to an irritant or allergen; may be itchy but not painful
- Fungal infections – redness and scaling in warm, moist areas like the groin or under the breasts; may have a ring-like pattern
- Scabies – intense itch and small bumps, especially in the finger webs, wrists, and genitals; highly contagious
A thorough evaluation by a dermatologist can help differentiate between these conditions and TSW. Patch testing may be recommended if contact dermatitis to the topical steroid or another ingredient is suspected.
Managing Topical Steroid Withdrawal
Currently, there is no cure or proven treatment for TSW. The main approach is to stop using the topical steroid and provide supportive care to ease symptoms while the skin heals and recovers. This process can take weeks, months, or even years, depending on the individual case[1].
Quitting Topical Steroids: Cold Turkey vs Tapering
One of the most challenging aspects of TSW is the initial decision to stop using topical steroids. Many people are understandably fearful of the worsening symptoms that can occur. There are two main approaches to quitting topical corticosteroids:
- Cold turkey – abruptly stopping all topical steroids at once
- Tapering – gradually reducing the potency and/or frequency of topical steroid use over time
The choice between cold turkey and tapering is an individual one that should be made with the guidance of a dermatologist. In general, studies suggest that cold turkey or a rapid taper (over a few weeks) may lead to shorter overall withdrawal symptoms compared to a slow taper over months to years[1]. However, some people may find a gradual taper easier to tolerate physically and emotionally.
Regardless of the approach, it’s crucial to have a plan in place for managing symptoms and flares during the withdrawal process. This may include:
- Moisturization – applying fragrance-free, hypoallergenic creams or ointments to soothe and protect the skin barrier
- Wet wraps – using damp clothing or gauze to hydrate and calm inflamed skin
- Antihistamines – taking oral medications like diphenhydramine or hydroxyzine to reduce itch and improve sleep
- Pain relief – using acetaminophen or other over-the-counter pain medications as needed for discomfort
- Stress management – practicing relaxation techniques, seeking counseling, and building a support network
It’s important to avoid using other topical steroids or systemic steroids during the withdrawal process as this can prolong or worsen symptoms. If there is concern about adrenal insufficiency from prolonged steroid use, an endocrinologist may need to be involved in the care team.
Skin Care During TSW
Gentle skin care is essential during TSW to prevent further irritation and promote healing. Some key tips include:
- Bathing – taking short, lukewarm baths or showers and avoiding hot water or harsh soaps that can dry and irritate the skin
- Moisturizing – applying thick, fragrance-free creams or ointments immediately after bathing and throughout the day as needed to combat dryness and itch
- Wet wraps – soaking gauze or clothing in warm water, applying to affected skin, and covering with dry material to boost hydration
- Avoiding triggers – identifying and eliminating potential irritants like fragrances, dyes, rough fabrics, sweat, and emotional stress
- Sun protection – wearing broad-spectrum sunscreen and protective clothing when outdoors to prevent further skin damage and hyperpigmentation
The National Eczema Association has a helpful list of moisturizers and cleansers that are suitable for sensitive skin during TSW[2]. Look for products with nourishing ingredients like ceramides, hyaluronic acid, and petrolatum to replenish the skin barrier.
Medications for TSW
While there is no FDA-approved medication for TSW, certain treatments may be used off-label to manage specific symptoms under the guidance of a dermatologist. These include:
- Topical calcineurin inhibitors – non-steroid medications like tacrolimus and pimecrolimus that can reduce inflammation and itch without causing skin thinning; may be helpful for face and genital area[2]
- Oral antibiotics – used to treat secondary bacterial skin infections that can occur due to skin breakdown and scratching
- Oral antihistamines – medications like diphenhydramine or cetirizine that can relieve itch and improve sleep
- Oral corticosteroids – rarely used in severe cases under close supervision to quickly control inflammation; can cause rebound symptoms when stopped[1]
- Immunosuppressants – medications like cyclosporine or methotrexate that suppress the immune system; reserved for severe, refractory cases[1]
The risks and benefits of any medication need to be carefully weighed, as some treatments have the potential for serious side effects. It’s important to follow the prescribing doctor’s instructions closely and report any adverse reactions.
Phototherapy for TSW
Narrowband UVB phototherapy is a treatment that uses artificial ultraviolet light to calm skin inflammation and speed healing. It is usually administered 2-3 times per week in a dermatologist’s office or with a home phototherapy unit[1].
Studies have found that narrowband UVB can be a helpful adjunct therapy for TSW, particularly for reducing itch and promoting skin healing. However, it may not be appropriate for everyone, especially those with very fair skin or a history of skin cancer.
If considering phototherapy, it’s important to go to an experienced provider and follow the recommended treatment plan. Consistency is key for optimal results.
Alternative and Complementary Therapies
Many people with TSW turn to alternative therapies to help manage their symptoms, though the evidence for their effectiveness is limited. Some options that may be worth discussing with a healthcare provider include:
- Acupuncture – may help reduce pain and itch by stimulating the release of endorphins and serotonin[1]
- Massage therapy – can promote relaxation and improve sleep quality
- Herbal remedies – certain herbs and supplements like aloe vera, calendula, and omega-3 fatty acids have anti-inflammatory and skin-soothing properties; should be used with caution as some can interact with medications[1]
- Mind-body practices – stress-reduction techniques like meditation, deep breathing, and yoga may help alleviate the emotional burden of TSW and promote a sense of well-being
It’s crucial to talk with a doctor before starting any alternative therapy, as some practices may not be safe or appropriate for everyone. Be sure to disclose all supplements and remedies being used to avoid potential interactions.
Coping with the Psychological Impact of TSW
The physical discomfort and visible skin changes of TSW can take a significant toll on mental health. It’s common for people to feel anxious, depressed, and isolated during the withdrawal process.
Some strategies that may help cope with the psychological challenges of TSW include:
- Seeking support – connecting with others who understand the experience through online forums like the ITSAN (International Topical Steroid Addiction Network) or in-person support groups
- Counseling – working with a therapist who specializes in chronic health conditions to develop coping strategies and process difficult emotions
- Stress management – engaging in activities that promote relaxation and reduce stress, such as deep breathing, progressive muscle relaxation, or mindfulness meditation
- Self-care – prioritizing activities that bring joy and a sense of accomplishment, such as reading, listening to music, spending time in nature, or pursuing a hobby
It’s important to remember that healing is not a linear process. There will be ups and downs, flares and remissions. Celebrating small victories and practicing self-compassion can help cultivate resilience during the tough times.
If feelings of depression, anxiety, or hopelessness become overwhelming, don’t hesitate to reach out for professional help. The National Suicide Prevention Lifeline (1-800-273-8255) and Crisis Text Line (text HOME to 741741) are available 24/7 for support.
Preventing Topical Steroid Withdrawal
The best way to prevent TSW is to use topical steroids appropriately and only as directed by a healthcare provider. Some key principles include:
- Using the lowest potency steroid needed to control symptoms
- Applying a thin layer to affected areas only, not on healthy skin
- Following the recommended frequency of application (usually once or twice daily)
- Not using for longer than 2-4 weeks continuously without a break
- Avoiding long-term use on sensitive areas like the face, genitals, and skin folds
When it is time to discontinue a topical steroid, it’s important to work with a doctor on a tapering plan to minimize the risk of withdrawal symptoms[1]. This may involve gradually reducing the potency and/or frequency of use over a period of weeks to months.
Parents and caregivers of children with eczema or other inflammatory skin conditions should be especially cautious with topical steroids. Overuse at a young age can have lasting impacts on skin health and increase the risk of TSW[2]. Close supervision and regular check-ins with a pediatric dermatologist are essential.
The Road to Recovery
Healing from topical steroid withdrawal is a highly individual journey that requires patience, support, and self-advocacy. It’s important to work closely with a knowledgeable dermatologist who can provide guidance and monitor progress over time.
While the process can be lengthy and challenging, most people do eventually recover and achieve healthy, resilient skin. Some may have lingering sensitivity or flares, but these tend to become less frequent and severe as time goes on[1].
In the meantime, it’s important to focus on self-care and symptom management. This may involve:
- Maintaining a gentle, fragrance-free skincare routine
- Wearing loose, breathable clothing to minimize irritation
- Keeping a journal to track triggers and flares
- Staying connected with supportive friends, family, and the TSW community
- Advocating for your needs with healthcare providers and loved ones
- Practicing stress-reduction techniques and engaging in enjoyable activities
- Celebrating small victories and progress along the way
As more research emerges on the mechanisms behind TSW and effective treatment strategies, there is hope for better prevention and management of this challenging condition. In recent years, the medical community has become increasingly aware of the potential for topical steroid withdrawal, thanks in large part to the advocacy efforts of TSW sufferers and organizations like ITSAN.
If you are currently going through TSW, know that you are not alone. There is a growing community of individuals who have been through the process and come out the other side. Don’t hesitate to reach out for support, whether through online forums, local support groups, or connecting with a therapist who understands chronic health conditions.
Remember, healing is not a linear process. There will be ups and downs, good days and bad days. Be patient with yourself and trust that with time and proper care, your skin will heal. Celebrate your strength and resilience in navigating this challenging journey.
Key Points
- Topical steroid withdrawal is a serious condition that can occur from prolonged, frequent, or inappropriate use of topical corticosteroids
- Common symptoms include burning, stinging, itching, and red skin that appears after stopping long-term topical steroids
- Diagnosis is based on a careful history and examination by a knowledgeable dermatologist
- Management involves discontinuing topical steroids, gentle skin care, and medications for specific symptoms like itch or infection; phototherapy may also be helpful
- The psychological impact of TSW can be significant, so it’s important to seek support from loved ones, the TSW community, and mental health professionals
- Most people with TSW eventually recover with time and proper care, though the process can be lengthy
- Topical steroids should be used judiciously and only as directed by a doctor to minimize the risk of withdrawal
- If you suspect you may have TSW, seek evaluation and care from a dermatologist familiar with the condition
Frequently Asked Questions
How long does topical steroid withdrawal last?
The duration of TSW varies from person to person, but symptoms can persist for weeks to months after stopping the medication. In some cases, full recovery may take 1-2 years. Working closely with a dermatologist can help manage symptoms and promote healing.
Can I use moisturizers or other treatments during topical steroid withdrawal?
Yes, gentle moisturizers and emollients can help soothe and protect the skin during TSW. Avoid products with fragrances, dyes, or other common irritants. Certain medications like topical calcineurin inhibitors or oral antihistamines may also be recommended for specific symptoms. Talk with your doctor about the best options for your situation.
Is TSW contagious?
No, TSW is not contagious. It is an individual reaction to the prolonged use of topical corticosteroids and cannot be spread from person to person.
Will my skin ever be the same after going through topical steroid withdrawal?
Most people who go through TSW do eventually achieve clear, healthy skin. However, some may have lingering sensitivity or occasional flares, especially during times of stress. Continuing with a gentle skincare routine and avoiding triggers can help maintain skin health long-term.
Are there any support resources for people going through TSW?
Yes, there is a growing community of individuals who have experienced TSW and offer support to others going through the process. The International Topical Steroid Addiction Network (ITSAN) is a helpful resource for connecting with others, finding local support groups, and accessing the latest research and treatment information. The National Eczema Association also offers resources and support for managing eczema and TSW.
If you suspect that you or a loved one may be experiencing topical steroid withdrawal, know that you are not alone. With proper care, support, and time, it is possible to navigate this challenging condition and achieve healthy, resilient skin. Don’t hesitate to reach out to a dermatologist or other healthcare provider for guidance on your journey to healing.
References
- Sheary, B. (2018). Topical steroid addiction and withdrawal-An overview for GPs. Australian family physician, 47(10), 668-671.
- Hajar, T., Leshem, Y. A., Hanifin, J. M., Nedorost, S. T., Lio, P. A., Paller, A. S., … & Simpson, E. L. (2015). A systematic review of topical corticosteroid withdrawal (“steroid addiction”) in patients with atopic dermatitis and other dermatoses. Journal of the American Academy of Dermatology, 72(3), 541-549.
- Juhász, M. L., Curley, R. A., Rasmussen, A., Malakouti, M., Silverberg, N., & Jacob, S. E. (2017). Systematic review of the topical steroid addiction and topical steroid withdrawal phenomenon in children diagnosed with atopic dermatitis and treated with topical corticosteroids. Journal of the Dermatology Nurses’ Association, 9(5), 233-240.
Related articles
Made in USA





