You May Be Interested In:
Cold plasma in dermatology represents a revolutionary non-invasive treatment modality transforming how clinicians approach inflammatory skin conditions, infectious diseases, wound healing, and cosmetic rejuvenation in 2025. Cold atmospheric plasma (CAP) generates ionized gas at safe temperatures (35-40°C) producing reactive oxygen and nitrogen species (RONS) that destroy bacteria, reduce inflammation, stimulate collagen production, and enhance skincare absorption by up to 24%[1]. Clinical trials demonstrate statistically significant improvements across multiple conditions: 99.9% acne bacteria elimination within 2-5 minutes, atopic dermatitis ADAS scores improving (p<0.001), and 88.1% of eczema patients reporting no itching after treatment[2].
This fourth state of matter technology operates through multiple therapeutic mechanisms simultaneously—antimicrobial action preventing antibiotic resistance, cytokine modulation reducing inflammation, fibroblast activation promoting tissue regeneration, and plasmaporation increasing topical medication penetration. With minimal side effects (<5% experience transient redness), no downtime, and safety across all Fitzpatrick skin types, cold plasma addresses the critical need for effective alternatives to medications causing systemic toxicity and laser treatments risking thermal damage.
Understanding Dermatology and Current Treatment Challenges
Common Dermatologic Conditions
Dermatologic diseases affect 30-50% of the US population at any given time, creating substantial medical and economic burdens[3]. Inflammatory skin diseases including acne, eczema (atopic dermatitis), psoriasis, and rosacea represent the most prevalent chronic conditions requiring ongoing management. Infectious conditions caused by bacteria (MRSA, Staphylococcus aureus), viruses (human papillomavirus causing warts), and fungi (onychomycosis affecting nails) challenge clinicians with increasing antimicrobial resistance.
Chronic wounds—diabetic foot ulcers, venous stasis ulcers, pressure sores, and burns—affect millions of patients annually with healing complications and infection risks. Skin cancer and precancerous lesions including actinic keratosis, basal cell carcinoma, and melanoma require effective treatments balancing efficacy with cosmetic outcomes. Aging and cosmetic concerns encompassing wrinkles, fine lines, skin laxity, and pigmentation disorders drive growing demand for non-invasive rejuvenation options.
Limitations of Traditional Dermatology Treatments
Conventional dermatology therapies face significant limitations constraining treatment outcomes and patient satisfaction. Systemic oral medications—antibiotics for acne, retinoids for psoriasis, immunosuppressants for severe inflammatory conditions—cause substantial side effects including gastrointestinal distress, liver toxicity, and immunosuppression requiring ongoing laboratory monitoring[3].
Critical treatment challenges include:
- Antibiotic resistance developing with prolonged topical and oral antimicrobial use
- Skin irritation and sensitivity from harsh topical agents (benzoyl peroxide, tretinoin)
- Limited efficacy for drug-resistant or chronic refractory conditions
- Thermal damage and pigmentation risks from laser and intense pulsed light (IPL) treatments
- Downtime and recovery requirements for ablative procedures (chemical peels, fractional lasers)
- Systemic absorption concerns with topical steroids causing skin atrophy and HPA axis suppression
These limitations create demand for innovative technologies offering comparable or superior efficacy without conventional treatment drawbacks. For comprehensive information on advanced treatment modalities, visit Mirari Doctor resources.
Economic and Quality of Life Impact
The dermatologic disease burden extends far beyond physical symptoms affecting psychological wellbeing, social functioning, and economic productivity. Annual US costs exceed $75 billion for acne, eczema, and psoriasis combined including direct medical expenses and indirect costs from lost work productivity[3].
Psychological consequences include decreased self-esteem, social anxiety, and clinical depression—particularly prevalent in adolescents with severe acne and adults with visible inflammatory conditions. Visible skin conditions create social stigma affecting relationships, employment opportunities, and overall quality of life. Treatment side effects from systemic medications further compound these challenges, creating cycles where therapies meant to improve conditions sometimes worsen overall wellbeing.
What Is Cold Plasma in Dermatology?
Definition and Scientific Principles
Cold atmospheric plasma represents ionized gas generated at near-room temperature (35-40°C) through electrical discharge applied to ambient air or noble gases including argon and helium[1]. This fourth state of matter—beyond solid, liquid, and gas—creates a cloud of charged particles, free radicals, reactive species, and ultraviolet radiation. The non-thermal nature enables direct skin contact without burns or thermal damage, distinguishing it fundamentally from thermal plasma used in industrial cutting and surgical applications operating at thousands of degrees.
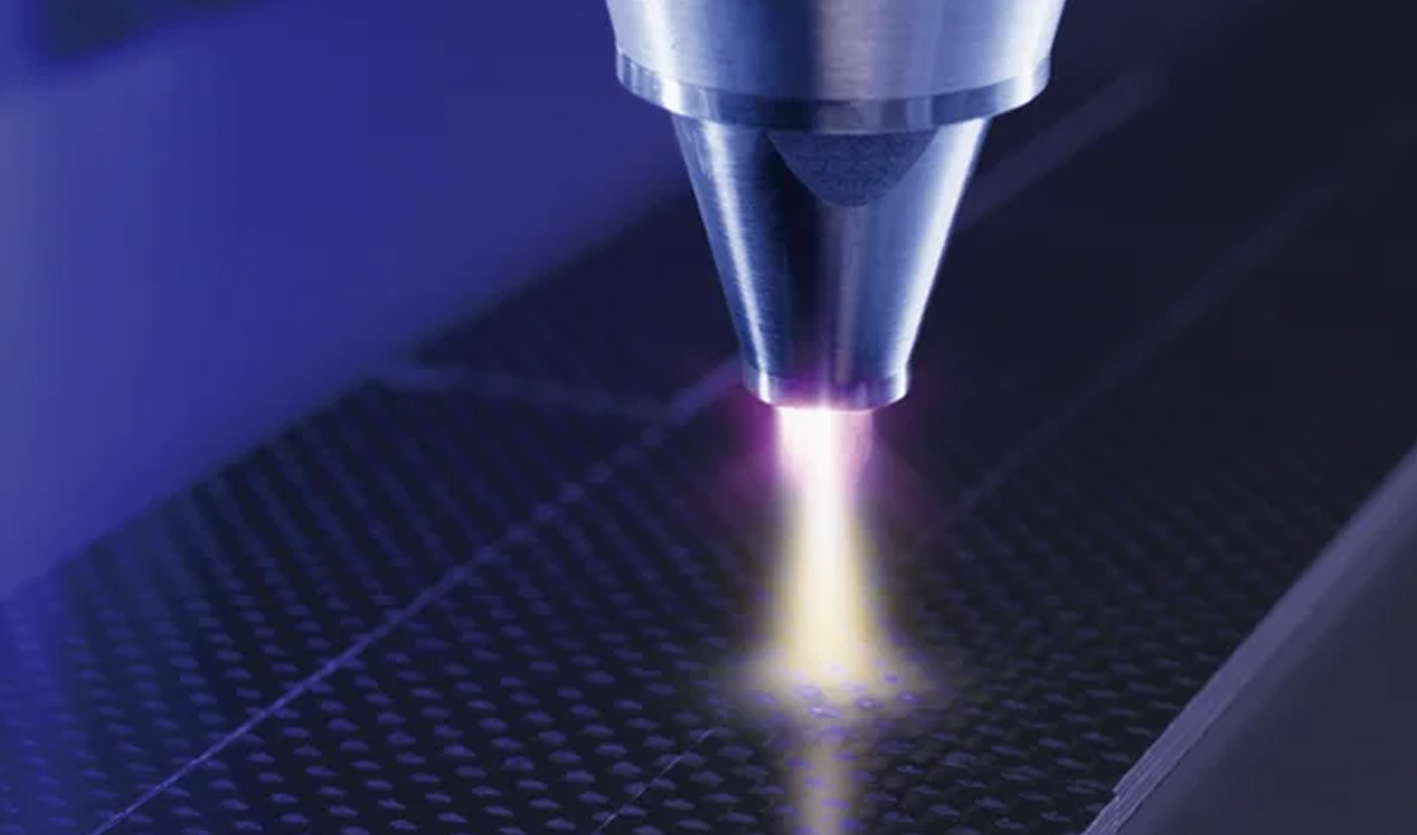
One pioneering device applying this technology is the Mirari Cold Plasma system, developed by General Vibronics and commercialized by Mirari Doctor. Unlike traditional ROS-based systems, it harnesses advanced radiofrequency integration for safe, non-thermal applications in dermatology, wound care, and pain management.
How Cold Plasma Works on Skin
The therapeutic mechanisms of cold plasma in dermatology stem from multiple coordinated biological effects occurring simultaneously[1][2]. The ionization process begins when electrical discharge transforms ambient gas into plasma containing reactive oxygen and nitrogen species (RONS) including hydrogen peroxide (H₂O₂), hydroxyl radicals (OH), nitric oxide (NO), peroxynitrite (ONOO⁻), and superoxide (O₂⁻).
Key therapeutic mechanisms:
- Plasmaporation: Cold plasma creates temporary microscopic pores in the stratum corneum (outermost skin layer), increasing permeability up to 24% and dramatically enhancing penetration of topical medications and active ingredients[1]. This effect persists for hours post-treatment, optimizing absorption of complementary skincare products.
- Temporary Oxidative Stress: The controlled generation of reactive species triggers beneficial biological signaling pathways without causing tissue damage. This mild oxidative environment activates cellular repair mechanisms, stimulates growth factor production, and modulates immune responses—all essential for tissue regeneration and inflammation resolution.
- UV Photon Emission: Cold plasma devices emit primarily safe UV-A spectrum radiation (310-470nm) contributing to antimicrobial effects and cellular activation while filtering harmful UV-B and UV-C wavelengths. This controlled UV exposure supplements the therapeutic effects of reactive species.
Therapeutic Mechanisms in Dermatology
Cold atmospheric plasma exerts multiple simultaneous therapeutic effects making it uniquely versatile across diverse dermatologic applications[2]. Understanding these mechanisms helps clinicians optimize treatment protocols for specific conditions.
| Mechanism | Biological Effect | Clinical Application | Timeframe |
|---|---|---|---|
| Antimicrobial Action | 99.9% bacterial/viral/fungal elimination | Acne, wound infections, warts | Minutes (2-5 min) |
| Anti-Inflammatory | TNF-α, IL-6, IL-1β reduction | Eczema, psoriasis, rosacea | Days to weeks |
| Tissue Regeneration | Collagen/elastin synthesis, angiogenesis | Anti-aging, wound healing | Weeks to months |
| Sebum Regulation | Normalizes oil production | Acne prevention | 2-4 weeks |
| Enhanced Absorption | 24% increased permeability | Topical medication efficacy | Hours post-treatment |
The antimicrobial action operates through multi-target inactivation destroying bacteria (Cutibacterium acnes, Staphylococcus aureus, MRSA), viruses (HPV, adenovirus), and fungi—critically preventing antimicrobial resistance development unlike antibiotics. Anti-inflammatory effects reduce pro-inflammatory cytokines while modulating immune responses, addressing the root cause of inflammatory dermatoses. For detailed information on cold plasma in dermatology, explore comprehensive clinical applications.
Clinical Applications in Dermatology
Acne Treatment
Cold plasma revolutionizes acne therapy through its multi-factorial approach addressing bacterial overgrowth, inflammation, and sebum dysregulation simultaneously[2][4]. Clinical validation from University Clinic Regensburg and Dermatest demonstrates 99.9% elimination of Cutibacterium acnes (formerly Propionibacterium acnes) within 2-5 minutes of application—the fundamental bacteria driving inflammatory acne pathogenesis.
Treatment benefits and protocols:
- Destroys acne bacteria through oxidative membrane damage without resistance development
- Regulates sebum production reducing oiliness and preventing comedone formation
- Decreases inflammatory lesions, redness, and swelling through cytokine modulation
- Suitable for teenage (age 12+ with parental consent) and adult acne across all severities
- Treatment frequency: Daily or 2-3 times weekly sessions of 5-10 minutes
- Visible results: Typically within 4 weeks of consistent treatment
- No systemic side effects unlike oral antibiotics or isotretinoin
The PHLAS device, adapted from Max-Planck-Institute research, represents the first consumer-grade cold plasma technology launched in the US market (2025) enabling daily home treatment for ongoing acne management.
Inflammatory Skin Conditions
Multiple randomized controlled trials establish cold atmospheric plasma efficacy across chronic inflammatory dermatoses with statistically significant improvements in validated outcome measures[2]. The immune modulation and anti-inflammatory mechanisms address underlying pathophysiology rather than merely suppressing symptoms.
- Atopic Dermatitis/Eczema: Clinical trials demonstrate remarkable improvements with ADAS (Atopic Dermatitis Antecubital Severity) scores showing p<0.001 significance, EASI (Eczema Area and Severity Index) improvements (p=0.002), and SCORAD (SCORing Atopic Dermatitis) reductions (p=0.001). Most impressively, 88.1% of patients report no itching after treatment—addressing the most distressing symptom affecting sleep and quality of life.
- Psoriasis: PASI (Psoriasis Area and Severity Index) score improvements, decreased plaque thickness, and reduced scaling occur through normalized keratinocyte proliferation and immune regulation. Cold plasma often combines with phototherapy for synergistic effects.
- Rosacea: Studies document erythema size reduction (p=0.041) and inflammatory lesion decrease (p=0.03-0.04) through vascular regulation and anti-inflammatory cytokine modulation. Patients report decreased flushing and improved skin texture.
- Topical Steroid Withdrawal (TSW): For patients experiencing severe rebound inflammation after discontinuing long-term topical steroids, cold plasma reduces redness without additional steroid exposure, accelerates barrier restoration, and supports skin healing through natural regenerative mechanisms.
Wound Healing and Skin Regeneration
Cold plasma demonstrates exceptional efficacy accelerating healing across acute and chronic wounds through simultaneous antimicrobial action and tissue regeneration stimulation[5]. The technology addresses multiple barriers to wound closure including infection, biofilm formation, and impaired cellular function.
Clinical outcomes in chronic ulcers:
- Diabetic foot ulcers: 92% complete healing with cold plasma versus 32% with standard care alone
- Venous stasis ulcers: Accelerated closure rates and reduced recurrence
- Pressure sores: 40-60% faster healing than conventional wound care
- Burns: Reduced healing time, decreased scarring, better cosmetic outcomes
- Post-surgical wounds: Lower infection rates, faster closure, improved scar quality
Mechanisms driving wound healing include bacterial load reduction (99.9% within 2-5 minutes), angiogenesis promotion through VEGF upregulation, collagen synthesis enhancement, keratinocyte migration acceleration for re-epithelialization, and stem cell differentiation supporting tissue regeneration. For specific wound healing applications and protocols, consult evidence-based resources.
Anti-Aging and Cosmetic Rejuvenation
Cold plasma provides non-invasive facial rejuvenation through collagen stimulation, cellular turnover enhancement, and microcirculation improvement—all without thermal damage or downtime[1]. The technology activates fibroblasts increasing synthesis of structural proteins essential for skin firmness and elasticity.
Anti-aging mechanisms and benefits:
- Collagen Types I and III production increases improving skin firmness
- Elastin synthesis enhances skin elasticity and resilience
- Fine lines and wrinkles reduce through dermal remodeling
- Skin texture, tone, and radiance improve from enhanced cellular turnover
- Facial tightening provides subtle lifting effects without surgery
- Hyperpigmentation and uneven tone improve through melanocyte regulation
- Microcirculation enhancement delivers oxygen and nutrients optimizing skin health
Treatment protocols typically involve weekly 10-15 minute sessions for 4-6 weeks achieving initial results, followed by quarterly maintenance treatments sustaining benefits long-term. Many patients notice improvements within 1-2 sessions with cumulative enhancement through repeated treatments.
Cold Plasma Dermatology Devices and Technology
Professional Clinical Devices
Medical-grade cold plasma systems offer higher power output, advanced features, and versatile applications suitable for clinical dermatology practice[4]. Device selection should consider FDA or CE clearance status, published clinical evidence, safety features, and treatment versatility.
- Dr. Platon Cold Plasma: Employs plasma shower technology generating uniform treatment fields, operates at tissue-safe 35-40°C, features adjustable intensity settings, and delivers 10-minute full facial treatments. Popular in European aesthetic clinics and dermatology practices.
- kINPen Med (Germany): CE-marked medical device extensively studied in clinical research, approved for various medical applications including dermatology. Primarily used in academic institutions and research settings with substantial published evidence supporting efficacy.
- MIRARI Cold Plasma System: FDA 510(k) cleared in November 2024 (K242553) as Class II medical device for cutting, coagulation, and soft tissue treatment. Integrates 80 kHz monopolar radiofrequency with cold atmospheric plasma generation offering dual modality applications across dermatology, wound care, and pain management.
Home-Use Consumer Devices
The democratization of cold plasma technology through consumer devices enables daily treatment and maintenance therapy at significantly lower costs than ongoing professional sessions. The PHLAS device represents the first consumer-grade cold plasma technology adapted from rigorous Max-Planck-Institute research and launched in the US market (2025).
Home device features and considerations:
- Cost: $300-$800 one-time investment versus $150-$350 per professional session
- Convenience: Daily treatment at home fitting seamlessly into existing skincare routines
- Safety: Built-in safeguards, automatic shut-off mechanisms, age 12+ suitability
- Effectiveness: Clinical validation for acne, redness, inflammation management
- Limitations: Lower power output than professional devices, best for maintenance therapy
- Hygienic design: Exchangeable tips preventing contamination, portable compact units
The optimal approach often combines initial professional treatment series (6-8 sessions) establishing therapeutic effect followed by home device maintenance preserving long-term benefits at lower cost.
Treatment Process and Patient Experience
Treatment Session Protocol
Cold plasma dermatology treatments follow standardized protocols ensuring consistent outcomes and patient safety. The process begins with thorough skin cleansing removing makeup, oils, and debris that could interfere with plasma-skin interaction. Device preparation involves powering on the unit, selecting appropriate settings based on condition and skin type, and verifying safety indicators function properly.
Application technique specifics:
- Systematic coverage ensuring complete treatment of target area
- 1-5mm distance maintained between plasma source and skin surface
- Slow continuous movement preventing prolonged exposure to any single location
- Session duration: 5-20 minutes depending on treatment area size and condition severity
- Patient sensation: Mild tingling or slight warmth, generally comfortable and painless
- Immediate effects: Possible mild redness resolving within minutes to hours, no downtime required
Post-treatment care enhances results and supports skin healing. Moisturizer application immediately after treatment capitalizes on enhanced absorption (24% increased permeability). Standard sun protection (SPF 30+) continues as routine precaution. Avoiding harsh exfoliants for 24 hours prevents excessive irritation. Hydration through adequate water intake supports optimal skin healing.
Expected Timeline and Results
Understanding typical response timelines helps set realistic patient expectations and optimize treatment protocols. Results vary by condition severity, skin type, treatment frequency, and individual healing capacity[2].
Treatment response timeframes:
- Immediate (during/after treatment): Possible mild redness (rare), comfortable sensation, no pain
- Short-term (1-7 days): Antimicrobial effects reducing infection, initial inflammation reduction
- Medium-term (2-4 weeks): Visible acne improvement, decreased redness, enhanced texture
- Long-term (1-3 months): Collagen remodeling producing firmness, continued condition improvement
- Maintenance: Ongoing sessions (weekly to monthly) for chronic conditions or anti-aging preservation
Acne typically shows visible improvement within 4 weeks of consistent treatment. Inflammatory conditions like eczema and rosacea often improve within 2-4 weeks. Anti-aging effects accumulate gradually with collagen remodeling continuing 2-3 months post-treatment series. Chronic conditions require ongoing maintenance treatments sustaining benefits long-term.
Safety Profile and Side Effects
Clinical Safety Data
Extensive clinical experience encompassing thousands of patient treatments establishes cold atmospheric plasma as remarkably safe with minimal adverse events[2][6]. The non-thermal operation maintaining surface temperatures below 40°C prevents burns and thermal injury—the primary safety concern with laser and light-based therapies.
Safety advantages:
- Non-ablative technology: No tissue destruction, scarring, or permanent damage
- Safe for all Fitzpatrick skin types (I-VI) without pigmentation or hyperpigmentation risk
- Suitable for pediatric patients age 12+ with appropriate parental consent
- No systemic absorption or toxicity concerns
- 93.6% of patients report completely painless treatment experience
- Zero serious adverse events documented in published clinical trials
The multi-year follow-up data confirms no delayed complications or long-term safety concerns. This exceptional safety profile makes cold plasma particularly valuable for sensitive skin patients unable to tolerate conventional treatments and for chronic conditions requiring extended therapy.
Reported Side Effects
When side effects occur, they remain minimal, transient, and self-limiting. The incidence of any adverse effects remains below 5% across clinical studies—substantially lower than conventional dermatology treatments.
Documented side effects (all mild and temporary):
- Transient redness: Mild erythema lasting minutes to hours in rare cases
- Slight tingling: Comfortable sensation during treatment, not described as painful
- Temporary itching: <5% incidence, resolves spontaneously without intervention
- No burns, blisters, or scarring reported with properly administered treatment
- No cumulative toxicity enabling safe long-term repeated use
Key Takeaways
- Cold plasma dermatology uses ionized gas at safe 35-40°C temperatures generating reactive species treating acne, eczema, psoriasis, wounds, and providing anti-aging benefits.
- Clinical trials demonstrate 99.9% acne bacteria elimination within 2-5 minutes, 88.1% eczema patients report no itching, and statistically significant improvements (p<0.001-0.04) across inflammatory conditions.
- Treatment enhances skincare absorption 24% through plasmaporation, operates painlessly with 93.6% patient satisfaction, requires no downtime, and suits all skin types without pigmentation risk.
- Professional treatments cost $150-$350 per session while home devices ($300-$800) enable daily maintenance therapy at lower long-term expense than conventional treatments.
- Safety profile exceeds conventional therapies: no burns, no antibiotic resistance, no systemic side effects, and <5% adverse event incidence limited to mild transient redness.
- FDA-cleared devices (MIRARI Cold Plasma K242553) and CE-marked systems (kINPen Med) establish regulatory acceptance for medical applications with expanding clinical indications.
- Multi-target mechanisms prevent drug resistance unlike antibiotics, making cold plasma ideal for chronic conditions requiring long-term management without cumulative toxicity.
Frequently Asked Questions
What is cold plasma and how does it work for skin conditions?
Cold atmospheric plasma is ionized gas generated at safe 35-40°C temperatures by applying electrical charge to ambient air or noble gases[1]. Creates reactive oxygen and nitrogen species (RONS) causing temporary oxidative stress triggering healing pathways. Destroys bacteria, reduces inflammation, stimulates collagen production, and enhances product absorption through plasmaporation creating microscopic pores. Non-thermal technology allows direct skin contact without burns through multiple mechanisms: antimicrobial action, cytokine modulation, fibroblast activation, and angiogenesis promotion.
Is cold plasma treatment safe for all skin types?
Yes, safe for all Fitzpatrick skin types (I-VI) without pigmentation or scarring risk[2]. Non-thermal operation (<40°C) prevents thermal injury unlike lasers requiring skin type considerations. 93.6% patients report painless treatment with minimal side effects. Suitable for sensitive skin unable to tolerate harsh topicals or procedures. Age 12+ appropriate with parental consent for minors. Contraindications minimal: pregnancy, implanted electronic devices near treatment area are primary precautions.
How effective is cold plasma for treating acne?
Eliminates 99.9% of Cutibacterium acnes (formerly P. acnes) within 2-5 minutes application[4]. Clinical trials show reduced redness, refined pores, fewer blemishes within 4 weeks. Regulates sebum production preventing future breakouts through normalized oil production. Anti-inflammatory effects decrease swelling and inflammatory lesions. No antibiotic resistance development unlike conventional therapies. Suitable for teenage and adult acne, all severity levels. Treatment protocol: Daily or 2-3 times weekly, 5-10 minutes per session produces visible improvement.
Can cold plasma treat eczema and psoriasis?
Atopic dermatitis demonstrates statistically significant ADAS (p<0.001), EASI (p=0.002), SCORAD (p=0.001) improvements in clinical trials[2]. Psoriasis shows PASI score reductions, decreased plaque thickness, reduced scaling. 88.1% eczema patients report no itching after treatment—the most distressing symptom. Mechanisms include immune modulation, anti-inflammatory cytokine reduction, barrier restoration. Treatment frequency: 2-3 times weekly initially, maintenance as needed. Safe alternative or complement to topical steroids without atrophy or rebound risks.
How much does cold plasma dermatology treatment cost?
Professional single session costs $150-$350 depending on geographic location and clinic type. Course of 6-8 treatments ranges $800-$2,400 with package discounts typically applied. Home devices cost $300-$800 one-time purchase. Annual maintenance costs $600-$1,500 for professional or home use versus $2,000-$5,000+ for conventional therapies. Insurance generally doesn’t cover treatments (considered cosmetic/elective). Cost-effectiveness superior to ongoing prescription medications and laser treatments long-term due to no recurring medication expenses.
What conditions can cold plasma treat in dermatology?
Acne (all severities, teenage and adult), inflammatory conditions (eczema, psoriasis, rosacea, seborrheic dermatitis, topical steroid withdrawal), infectious diseases (bacterial including MRSA and S. aureus, viral warts, fungal infections including onychomycosis), wounds (diabetic ulcers, pressure sores, burns, post-surgical wounds), anti-aging concerns (fine lines, wrinkles, skin laxity, pigmentation), skin cancer (actinic keratosis, basal cell carcinoma with approved devices), and hair loss conditions (alopecia)[1][2].
How long do cold plasma treatment results last?
Antimicrobial effects provide immediate bacterial reduction lasting days. Acne improvement becomes visible within 4-8 weeks requiring maintenance for ongoing control. Anti-aging effects from collagen remodeling continue 2-3 months post-treatment with cumulative results through repeated sessions. Wound healing accelerates closure with sustained effects through complete healing. Chronic conditions (eczema, psoriasis, rosacea) require ongoing maintenance treatments (weekly to monthly). Longevity varies by condition severity, skin type, lifestyle factors, and maintenance treatment adherence.
Are there any side effects from cold plasma facial treatments?
Minimal side effects with <5% experiencing any adverse effects. Transient redness (mild erythema) resolves within minutes to hours in rare occurrences. Slight tingling during treatment described as comfortable, not painful. No burns, blisters, or scarring reported with properly administered treatments. No downtime required—immediate return to activities including makeup application. No cumulative toxicity enabling safe long-term repeated use. Serious adverse events: zero documented in extensive clinical trials[6].
Can I use cold plasma at home or do I need professional treatment?
Home devices available including PHLAS and similar consumer devices ($300-$800) FDA-registered for cosmetic use. Professional advantages include medical-grade devices, higher power, expert application, better results for severe conditions. Home use benefits: daily convenience, lower long-term cost, maintenance therapy, privacy. Optimal approach: initial professional series (6-8 sessions) establishing therapeutic effect followed by home device maintenance. Safety: both home and professional devices safe with proper use and built-in safeguards. Results: professional treatments provide faster initial improvement; home devices effective for maintenance.
How does cold plasma compare to laser treatments for skin?
Cold plasma offers superior safety—no burns, pigmentation changes, or thermal damage; suitable for all skin types[1]. Downtime: cold plasma none versus lasers 3-14 days depending on intensity. Mechanism: cold plasma RONS-based versus lasers heat-based selective photothermolysis. Pain: cold plasma painless versus lasers requiring numbing for many procedures. Cost: cold plasma $150-$350/session versus lasers $400-$1,500/session. Applications: cold plasma treats infections (lasers cannot); lasers better for deep vascular/pigmented lesions. Versatility: single cold plasma device treats multiple conditions; lasers condition-specific.
References
- Friedman PC. (2023). Cold Plasma in Dermatology: Clinical Uses and Future Directions. The Derm Learning Network. https://www.hmpgloballearningnetwork.com/site/thederm/practice-advances/cold-plasma-dermatology-clinical-uses-and-future-directions
- Riopel D, Phillips N. (2025). Cold Atmospheric Plasma in Inflammatory and Infectious Skin Diseases: A Review. Journal of Integrative Dermatology. https://jintegrativederm.org/doi/10.64550/joid.hhwhg996
- American Academy of Dermatology. (2025). Skin Conditions Statistics. AAD Public Resource Center. https://www.aad.org/media/stats-numbers
- Farkas A. (2025). Revolutionizing Acne Treatments and Skin Care with Cold Plasma Technology. Dermatology Times. https://www.dermatologytimes.com/view/revolutionizing-acne-treatments-and-skin-care-with-cold-plasma-technology
- Strohal R, Mittlböck M, Gebhardt L, Hämmerle G. (2025). Treatment of chronic wounds with cold plasma: a randomised, single-blind, placebo-controlled clinical study. Journal of Wound Care. 34(8):542-554. https://www.magonlinelibrary.com/doi/10.12968/jowc.2025.0207
- Wang J, Zhang X, Li Y, et al. (2025). Efficacy and Safety of Cold Atmospheric Plasma-Assisted Therapy for Herpes Zoster: A Randomized, Parallel, Positive-Controlled, Non-inferiority Trial. Dermatology and Therapy. https://pubmed.ncbi.nlm.nih.gov/40601233/
Related articles
Made in USA