Back pain affects millions of people worldwide, representing one of the most common reasons for medical visits and disability claims. This pervasive condition impacts individuals across all age groups, from young adults experiencing acute muscle strains to elderly patients dealing with chronic degenerative conditions[1]. Understanding back pain’s complex nature—from acute episodes lasting days to chronic conditions persisting for months—is crucial for effective treatment selection. Revolutionary cold atmospheric plasma technology is now offering patients an innovative, non-invasive alternative that addresses back pain through unique biological mechanisms, providing hope for those seeking relief beyond traditional pharmaceutical and surgical interventions.
Understanding Back Pain: Causes, Types, and Impact
Back pain encompasses a broad spectrum of conditions affecting the spine’s complex anatomical structures, including vertebrae, intervertebral discs, ligaments, muscles, and nerves[2]. The condition can originate from mechanical problems, inflammatory processes, or other medical conditions that affect spinal structures.
Acute vs Chronic Back Pain: Critical Distinctions
The classification of back pain into acute and chronic categories fundamentally influences treatment approaches and patient outcomes. Acute back pain typically develops suddenly and lasts less than a few weeks, often resulting from identifiable incidents such as lifting injuries, sudden movements, or muscle strains[3]. This type of back pain generally responds well to conservative treatment and resolves without permanent functional impairment.
Chronic back pain persists for 12 weeks or longer, often continuing even after the initial injury has healed[3]. Unlike acute conditions, chronic back pain involves complex neurological changes that perpetuate discomfort and may include conditions such as degenerative disc disease, spinal stenosis, arthritis, and fibromyalgia.
Common Causes of Back Pain
Mechanical and structural problems represent the most frequent causes of back pain. These include sprains affecting spinal ligaments, strains involving muscles or tendons, and degenerative disc disease where aging causes discs between vertebrae to break down[4]. Herniated discs, spondylolisthesis, and spinal stenosis also contribute significantly to back pain prevalence.
Inflammatory conditions such as ankylosing spondylitis and other types of inflammatory arthritis can cause persistent back pain[4]. Additional medical conditions including osteoporosis, fibromyalgia, kidney stones, infections, and rarely tumors can also manifest as back pain.
Risk Factors and Prevention Strategies
Several modifiable and non-modifiable factors increase back pain susceptibility. Lack of exercise leading to weak, unused muscles in the back and abdomen significantly contributes to back pain development[1]. Excess body weight puts additional stress on spinal structures, while poor posture during daily activities creates mechanical strain.
Occupational factors including heavy lifting, prolonged sitting, and exposure to vibration increase back pain risk. Age-related changes, genetic predisposition, and psychological factors such as stress and depression also influence back pain development and persistence[5].
Revolutionary Cold Plasma Technology for Back Pain Relief
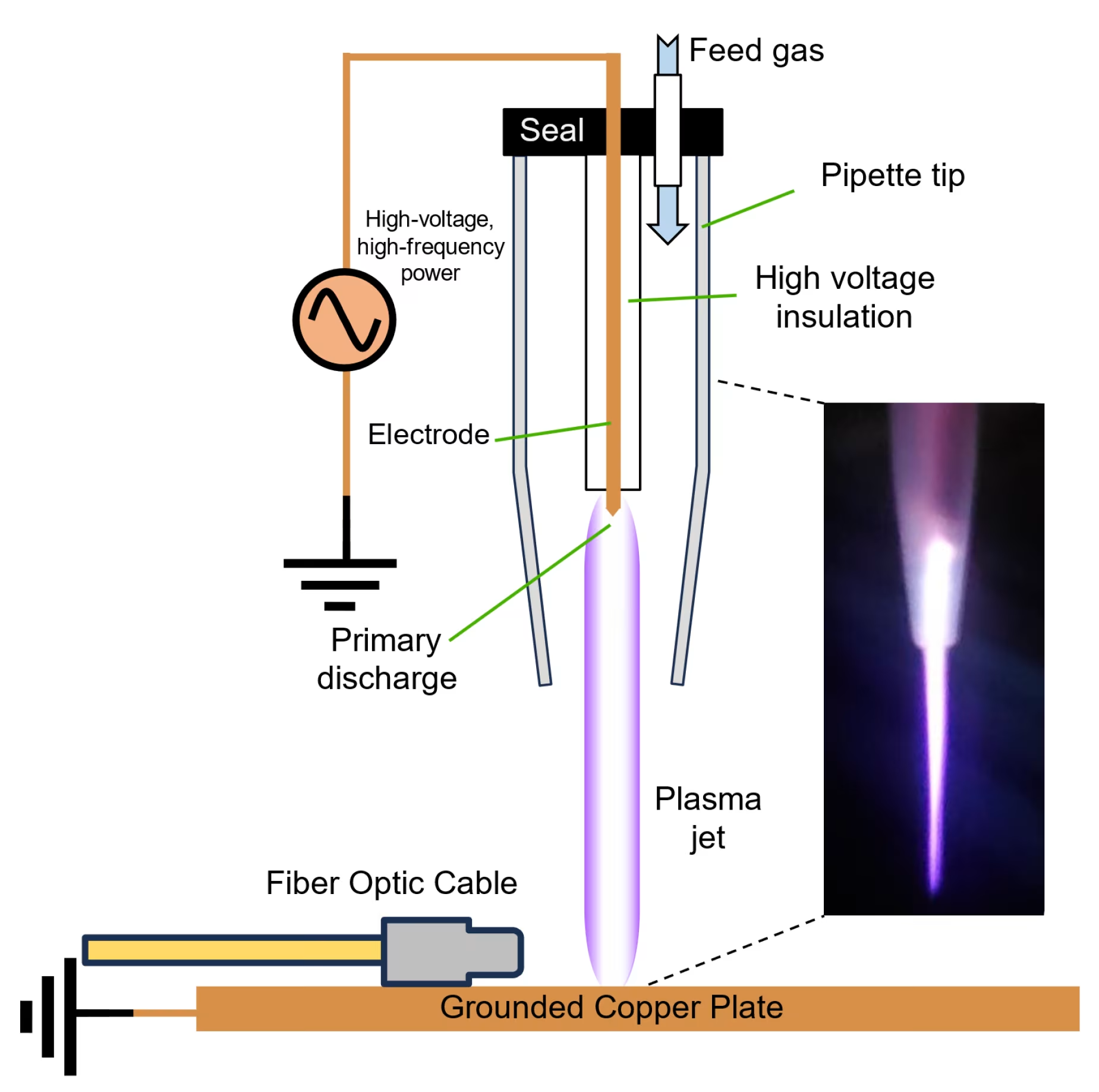
Cold atmospheric plasma represents a groundbreaking advancement in back pain management, offering a non-invasive alternative that addresses pain through unique biological mechanisms. This innovative technology generates reactive oxygen and nitrogen species (RONS) at room temperature, creating therapeutic effects without thermal tissue damage[6].
Scientific Mechanisms Behind Cold Plasma Back Pain Treatment
Cold plasma therapy works through multiple pathways that benefit back pain conditions. The technology generates nitric oxide and other reactive species that modulate inflammatory mediators, improve microcirculation, and activate cellular repair processes[6]. These mechanisms directly address underlying causes of back pain rather than merely masking symptoms.
The MIRARI® Cold Plasma System, developed by General Vibronics and FDA-cleared in November 2024, represents a significant advancement in making this technology accessible for back pain treatment[7]. This handheld device utilizes nitric oxide-enriched plasma delivery, offering enhanced precision in targeting specific pain pathways.
Nitric Oxide vs Traditional Pain Management Approaches
Unlike traditional pain medications that may cause systemic side effects, cold plasma provides localized treatment through nitric oxide pathway modulation. Nitric oxide serves as a signaling molecule that can alter pain perception and transmission while promoting tissue healing[6]. This approach offers several advantages over conventional pharmaceutical interventions.
The MIRARI® system’s innovation lies in its nitric oxide-enriched plasma technology, which penetrates tissues more effectively than traditional delivery methods, creating sustained therapeutic effects for back pain relief[6].
Technical Specifications for Back Pain Applications
| Parameter | Specification | Clinical Significance |
|---|---|---|
| Operating Frequency | 80 kHz | Resonant plasma generation for stable, non-thermal operation |
| Power Output | Less than 4W | Low power ensures safety while delivering therapeutic effects |
| Treatment Duration | 10-15 minutes per session | Optimized for inflammation reduction and pain relief |
| Temperature Control | ±2°C tolerance (max 43°C) | Prevents thermal injury while achieving analgesic benefits |
| Plasma Array Size | 2.5 × 1.72 inches | Covers targeted back pain areas effectively |
| Patient Contact Material | 300 g/m² polyester fleece | Ensures even heat distribution and electrical insulation |
Clinical Applications of Cold Plasma in Back Pain Management
Cold plasma technology demonstrates versatility in treating various types of back pain, from acute muscle strains to chronic degenerative conditions. The therapy’s multi-modal approach addresses inflammation, promotes healing, and provides direct analgesic effects.
FDA-Cleared Technology for Back Pain Relief
The FDA clearance of the MIRARI® Cold Plasma System for heating tissue to elevate temperature validates its use in pain management applications[7]. The device provides heating for temporary relief of pain, muscle spasms, and increased local circulation, representing a significant milestone in establishing cold plasma as a legitimate therapeutic option for back pain patients.
Clinical applications include acute back injuries where rapid pain relief and tissue healing are priorities, chronic conditions requiring ongoing pain management, and post-surgical scenarios where enhanced recovery is desired[6]. The technology’s safety profile makes it suitable for diverse patient populations, including those who cannot tolerate conventional treatments.
Real-World Patient Outcomes in Back Pain Treatment
Clinical observations report several benefits from cold plasma treatment for back pain, including reduced pain intensity within a few sessions, improved mobility and function in daily activities, decreased reliance on pain medications, better sleep quality as pain diminishes, and enhanced quality of life with return to normal activities[6].
Case examples illustrate the technology’s potential: patients with acute back pain from muscle strains experienced significant pain reduction after daily 15-minute sessions for 1-2 weeks, achieving approximately 70% pain reduction[6]. Chronic lower back pain patients receiving treatments 3 times weekly for 4-6 weeks reported sustained pain relief and improved functional capacity.
Specific Back Pain Conditions Responding to Cold Plasma
The technology shows particular promise for several back pain conditions. Herniated disc pain responds to cold plasma therapy’s anti-inflammatory effects, which help reduce inflammation around affected nerve roots while promoting tissue healing[6]. Muscle-related back pain benefits from the system’s ability to modulate muscle spasms and promote tissue repair.
Neuropathic back pain responds to cold plasma’s capacity to modulate peripheral nervous system activity, helping reduce nerve excitability linked to chronic pain signal transmission[6]. The therapy’s multiple therapeutic pathways make it effective for complex back pain conditions involving various tissue types.
Clinical Benefits and Treatment Protocols
| Back Pain Type | Treatment Protocol | Session Duration | Expected Outcomes | Evidence Level |
|---|---|---|---|---|
| Acute Muscle Strain | Daily sessions for 1-2 weeks | 15 minutes | 70% pain reduction | Clinical observation |
| Chronic Lower Back Pain | 3x/week for 4-6 weeks | 15 minutes | Sustained pain relief | Case series |
| Muscle Spasms | 2x/day during acute phase | 10-15 minutes | Rapid spasm resolution | Clinical experience |
| Post-surgical Pain | Daily sessions post-op | 15 minutes | Reduced analgesic needs | Preliminary studies |
| Neuropathic Pain | Regular maintenance protocol | 15 minutes | Nerve signal modulation | Clinical reports |
Comparing Cold Plasma to Traditional Back Pain Treatments
Cold plasma offers distinct advantages over conventional back pain therapies through its comprehensive therapeutic mechanisms and excellent safety profile.
Non-invasive Benefits for Back Pain Patients
Unlike surgical interventions that require incisions and lengthy recovery periods, cold plasma provides immediate, non-invasive treatment options. The technology eliminates risks associated with general anesthesia, surgical complications, and extended downtime while offering effective pain relief[^8].
Compared to long-term medication use, cold plasma avoids potential side effects including gastrointestinal complications from NSAIDs, dependency risks from opioids, and systemic effects from prolonged pharmaceutical interventions. The localized nature of treatment ensures targeted therapy without affecting other body systems.
Safety Profile and Side Effects in Back Pain Applications
Clinical studies demonstrate excellent safety profiles for cold plasma in back pain applications. The technology operates at controlled temperatures and includes multiple safety features to protect patients during treatment[6]. Common side effects are minimal and typically limited to mild skin sensations that resolve quickly after sessions.
The non-thermal nature of cold plasma eliminates burn risks associated with other energy-based therapies, while the absence of ionizing radiation makes it suitable for repeated treatments without cumulative exposure concerns.
Integration with Comprehensive Back Pain Management
The MIRARI® Cold Plasma System, available through Mirari Doctor (miraridoctor.com), serves as an excellent adjunct therapy to traditional management strategies, including physical therapy, exercise, and lifestyle modifications. This integration approach maximizes therapeutic benefits while addressing multiple aspects of back pain pathophysiology[6].
Lifestyle Modifications and Prevention Strategies for Back Pain
Effective back pain management extends beyond clinical treatments to include comprehensive lifestyle modifications that address underlying risk factors and promote long-term spinal health.
Exercise and Physical Activity for Back Pain Prevention
Regular physical activity represents one of the most effective strategies for back pain prevention and management. Core strengthening exercises build muscular support for the spine, while low-impact aerobic activities improve cardiovascular health without stressing the back[5]. Flexibility exercises such as yoga and stretching routines enhance range of motion and reduce injury risk.
Walking, swimming, and gentle yoga provide excellent options for individuals with back pain, offering therapeutic benefits while maintaining fitness levels. These activities can be safely combined with cold plasma treatments to optimize overall outcomes.
Ergonomic Considerations and Posture Improvement
Poor posture contributes significantly to back pain development and persistence. Workplace ergonomics, proper lifting techniques, and maintaining neutral spine alignment during daily activities all play crucial roles in back pain prevention[5]. Ergonomic desk setups, supportive seating, and regular position changes help reduce occupational back pain risks.
Examples of postures that may eventually cause pain include forward head posture, slouching with rounded shoulders, and hyperlordosis where hips tilt forward, arching the lower back[5]. Everyday activities like driving, using computers positioned too low, and sleeping on unsupportive mattresses can contribute to postural problems.
Patient Selection and Treatment Planning for Back Pain
Successful cold plasma therapy requires appropriate patient selection and individualized treatment planning. Ideal candidates include patients with acute back injuries requiring rapid pain relief, individuals with chronic conditions seeking alternatives to medications, post-surgical patients requiring enhanced recovery support, and those seeking non-invasive treatment options[6].
Treatment Planning and Monitoring for Back Pain
Treatment planning considers pain location, intensity, duration, and underlying causes to develop optimal protocols. Healthcare providers assess individual patient factors to determine appropriate session frequency, treatment duration, and integration with other therapeutic modalities.
Regular assessment of treatment response ensures optimal outcomes and allows for protocol adjustments as needed. Parameters include pain intensity ratings, functional improvement measures, medication usage changes, and quality of life assessments[6].
Contraindications and Safety Considerations
Absolute contraindications include implanted pacemakers or metal implants in the treatment area, pregnancy, active malignancy in the treatment region, and severe coagulation disorders[6]. Relative contraindications include uncontrolled diabetes, open wounds in the treatment area, acute infection, and recent surgical procedures depending on timing.
Frequently Asked Questions
How quickly can patients with back pain expect relief from cold plasma therapy?
Clinical observations indicate that many patients experience noticeable pain reduction within the first few treatment sessions. Unlike medications that may take days to reach therapeutic levels or physical therapy that requires weeks for improvement, cold plasma often provides immediate analgesic effects during and immediately following treatment[6]. The technology’s ability to modulate pain pathways through nitric oxide delivery creates rapid onset of relief while simultaneously promoting tissue healing for sustained benefits.
Is cold plasma therapy safe for patients with chronic back pain who take multiple medications?
Cold plasma therapy demonstrates excellent safety profiles and shows no known contraindications with common back pain medications including NSAIDs, muscle relaxants, or prescription pain medications[6]. The localized, non-systemic nature of cold plasma treatment eliminates concerns about drug interactions while potentially allowing patients to reduce their medication requirements over time as pain improves through the therapy’s healing mechanisms.
Can cold plasma therapy be used for both acute and chronic back pain conditions?
Yes, cold plasma technology provides benefits for both acute and chronic back pain through its multi-modal therapeutic approach. For acute conditions, the therapy accelerates tissue healing and provides immediate pain relief, potentially preventing progression to chronic conditions[6]. In chronic back pain management, cold plasma helps modulate sensitized nerve pathways, reduces ongoing inflammation, and promotes tissue regeneration that addresses underlying pathological processes.
How does cold plasma therapy compare to physical therapy for back pain treatment?
Cold plasma therapy and physical therapy serve complementary roles in comprehensive back pain management rather than competing approaches. While physical therapy focuses on strengthening muscles, improving posture, and teaching movement patterns over weeks to months, cold plasma provides immediate pain relief and tissue healing that can enhance a patient’s ability to participate effectively in physical therapy exercises[6]. Many patients find the combination more effective than either therapy alone.
What types of back pain respond best to cold plasma treatment?
Cold plasma therapy shows effectiveness across various back pain conditions, with particularly strong responses seen in inflammatory conditions, muscle strains and spasms, nerve-related pain, and post-surgical recovery scenarios[6]. The technology’s ability to reduce inflammation, promote tissue healing, and modulate pain pathways makes it versatile for different underlying causes of back pain. Patients with acute injuries often see rapid improvements, while those with chronic conditions typically experience gradual but sustained benefits with regular treatments.
Conclusion
Back pain represents one of the most significant healthcare challenges of our time, affecting millions of people globally and creating substantial economic burdens for individuals and healthcare systems. While traditional treatment approaches have provided valuable therapeutic options, the introduction of cold atmospheric plasma technology offers a revolutionary advancement in back pain management.
The MIRARI® Cold Plasma System exemplifies how innovative medical technology can address the complex challenges of back pain through scientifically-based, non-invasive approaches. By harnessing the therapeutic power of nitric oxide-enriched plasma, this technology provides immediate pain relief while promoting long-term tissue healing and recovery.
As healthcare continues to evolve toward personalized, evidence-based treatments that prioritize patient safety and effectiveness, cold plasma therapy represents a significant step forward in back pain management. The technology’s excellent safety profile, immediate therapeutic effects, and compatibility with existing treatments position it as a valuable addition to comprehensive pain management protocols.
For patients struggling with back pain, whether acute or chronic, cold plasma therapy offers hope for improved outcomes, reduced reliance on medications, and enhanced quality of life. As research continues to expand our understanding of this technology’s mechanisms and optimize treatment protocols, cold plasma therapy will likely play an increasingly important role in transforming how we approach back pain management in the modern healthcare era.
References
- Mayo Clinic. (2024). Back pain – Symptoms and causes. https://www.mayoclinic.org/diseases-conditions/back-pain/symptoms-causes/syc-20369906
- Cleveland Clinic. (2025). Back Pain Causes, Treatment \& Pain Relief. https://my.clevelandclinic.org/health/symptoms/back-pain
- Alliance Ortho. (2024). From Acute to Chronic: Understanding Different Types of Back Pain. https://allianceortho.com/from-acute-to-chronic-understanding-different-types-of-back-pain/
- NIAMS. (2025). Back Pain Symptoms, Types, \& Causes. https://www.niams.nih.gov/health-topics/back-pain
- Medical News Today. (2025). What is causing my back pain, and how can I remedy it? https://www.medicalnewstoday.com/articles/172943
- Mirari Doctor. (2025). Back Pain Relief: A Complete Guide to Mirari Cold Plasma. https://miraridoctor.com/back-pain/
- FDA. (2024). 510(k) Summary – Mirari Cold Plasma System K242553. https://www.accessdata.fda.gov/cdrh_docs/pdf24/K242553.pdf
- Peak Chiropractic. (2025). Managing Back Pain: New Trends in 2025. https://peakportland.com/managing-back-pain-new-trends-in-2025/
Related articles
Made in USA