What is a diabetic foot ulcer? A diabetic foot ulcer is a breakdown of the skin and sometimes deeper tissues of the foot that leads to open sore formation[1]. These wounds represent one of the most serious complications of diabetes, affecting approximately 15% of patients with diabetes and serving as the leading cause of non-traumatic lower extremity amputations in the United States[2].
Understanding diabetic foot ulcers is crucial for anyone living with diabetes. These seemingly minor wounds can escalate into life-threatening conditions if left untreated, making early recognition and proper management essential for preserving both limbs and lives.
Understanding Diabetic Foot Ulcers: The Medical Reality
What Makes Diabetic Foot Ulcers So Dangerous?
Diabetic foot ulcers develop through a complex interplay of factors unique to diabetes. The condition occurs due to abnormal pressure or mechanical stress chronically applied to the foot, combined with predisposing conditions such as peripheral sensory neuropathy, peripheral motor neuropathy, autonomic neuropathy, or peripheral arterial disease[1].
The danger lies in the silent progression of these wounds. Many diabetic patients develop neuropathy, which reduces or completely eliminates the ability to feel pain in the feet due to nerve damage caused by elevated blood glucose levels over time[2]. This means patients often don’t notice when a simple blister, corn, or cut develops into a serious ulcer.
The Pathophysiology Behind Diabetic Foot Ulcers
A key feature of normal wound healing is the stepwise repair of lost extracellular matrix (ECM), the largest component of the dermal skin layer. However, in diabetic wounds, physiological insult from diabetes mellitus impedes this healing process[1].
The inflammatory phase of healing becomes prolonged in diabetic patients, delaying the formation of mature granulation tissue and reducing the healing wound’s tensile strength. This creates a perfect storm where minor injuries become chronic, non-healing wounds that can progress to life-threatening infections.
What Does a Diabetic Foot Ulcer Look Like? Visual Recognition Guide
Early Stage Appearance
Recognizing what a diabetic foot ulcer looks like in its early stages can save lives. Initial signs include:
- Discoloration: The skin around the foot ulcer may become discolored, turning red, dark blue, or purple, signifying inflammation or compromised blood flow[3].
- Foot Wounds: Any foot wound can signify early signs of a foot ulcer, including blisters, cuts, ingrown toenails, athlete’s foot, corns, or calluses[3].
- Swelling: Unusual swelling and redness around the wound area, often accompanied by a warm sensation close to the affected area[4].
Advanced Stage Characteristics
In advanced stages, a foot ulcer looks like a round red crater in the skin bordered by thickened callused skin. Severe ulcers can be deep enough to expose tendons or bones[4].
The most visible sign of a serious foot ulcer is black tissue (called eschar) surrounding the ulcer, which forms because of an absence of healthy blood flow to the area. Partial or complete gangrene may appear around the ulcer, accompanied by odorous discharge, pain, and numbness[5].
Warning Signs That Require Immediate Medical Attention
One of the first signs of a foot ulcer is drainage from your foot that might stain your socks or leak out in your shoe. Unusual swelling, irritation, redness, and odors from one or both feet are also common early symptoms[5].
Can You Die from Diabetic Foot Ulcer? Understanding the Mortality Risk
The Stark Reality of Diabetic Foot Ulcer Mortality
Can you die from diabetic foot ulcer? Yes, if not appropriately managed, diabetic foot ulcers can lead to serious infections, major amputations, and even death[6]. The mortality statistics are alarming and comparable to some forms of cancer.
Research shows that individuals with diabetic foot ulcers are at high risk of death in the short term, with one-third actually dying within three years of developing this common diabetes complication[7]. The five-year mortality rate for people with new-onset diabetic foot ulcers often mirrors those related to cancers like breast or prostate cancer.
Factors Contributing to Mortality Risk
Several critical factors influence mortality rates in diabetic foot ulcer patients:
| Risk Factor | Impact on Mortality |
|---|---|
| Duration of Diabetes | Increased risk with longer diabetes duration |
| Cardiovascular Disease | Elevates mortality risk significantly |
| Chronic Kidney Disease | Substantial increase in death risk |
| History of Foot Ulcers | Higher risk of recurrence and complications |
| Peripheral Neuropathy | Increased risk of severe complications |
About 30% of patients with diabetic foot ulcers died after three years in clinical studies. More than half of the deaths (52%) were due to infections, namely pneumonia (25%), followed by cardiovascular diseases and malignant diseases with 22% and 8%, respectively[7].
How to Treat Diabetic Foot Ulcer: Evidence-Based Medical Approaches
The Gold Standard Treatment Protocol
The gold standard for diabetic foot ulcer treatment includes debridement of the wound, management of any infection, revascularization procedures when indicated, and off-loading of the ulcer[8].
- Debridement: This critical procedure removes dead skin and tissue. Healthcare providers clean and disinfect the surrounding skin, probe the wound to assess depth and foreign material, then cut away dead tissue and wash out the ulcer[9].
- Off-loading: Keep pressure off your ulcer, especially if it’s on your foot. This may mean using crutches, special footwear, a brace, or other devices. A foot ulcer can’t heal if you put weight on the area[10].
Advanced Treatment Modalities
Modern diabetic foot ulcer treatment incorporates several advanced therapies:
- Antibiotic Treatment: For infected ulcers, targeted antibiotic therapy is essential. Broad-spectrum antibiotics such as cilastatin, levofloxacin, ciprofloxacin, cefuroxime, and ampicillin have shown effectiveness against severe diabetic foot infections[11].
- Hyperbaric Oxygen Therapy: This treatment helps deliver more oxygen to the wound, promoting healing in selected cases[9].
- Advanced Wound Care Products: Including growth factors, ulcer dressings, and skin substitutes that have shown high effectiveness in healing foot ulcers[2].
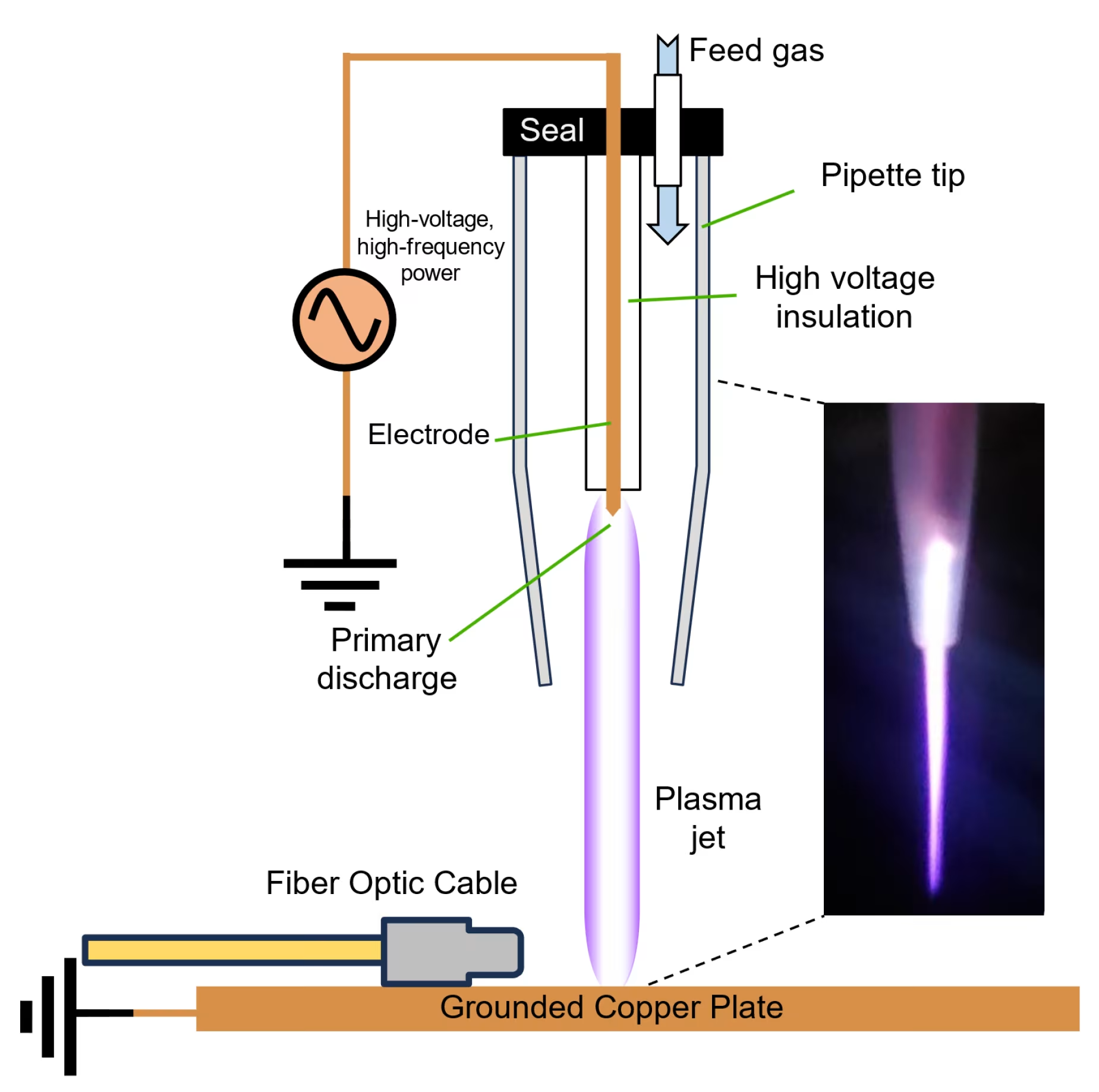
Innovative Cold Plasma Therapy
One of the pioneering medical devices applying cold plasma therapy for wound healing is the Mirari Cold Plasma system, developed by General Vibronics and brought to market by Mirari Doctor. This innovative device utilizes Nitric Oxide (NO) instead of traditional ROS-based systems to promote safe, non-thermal healing.
The Mirari Cold Plasma system represents a breakthrough in diabetic foot ulcer treatment by:
- Generating reactive oxygen and nitrogen species that stimulate wound healing
- Providing antimicrobial action without thermal damage
- Promoting tissue regeneration through controlled plasma application
- Offering a non-invasive alternative to traditional surgical interventions
How to Treat Diabetic Foot Ulcer at Home: Safe Self-Care Strategies
Essential Home Care Protocols
While professional medical care is crucial, proper home care plays a vital role in diabetic foot ulcer healing:
- Daily Wound Care: Clean your ulcer daily with soap and water, unless your doctor recommends another cleanser. Don’t use hydrogen peroxide or soak your wound in a bath, as this could reduce healing and increase infection risk[11].
- Blood Sugar Control: Keep your blood sugar level under good control. Tight glucose control is of utmost importance during treatment and enhances healing while reducing complication risk[2].
- Proper Bandaging: Keep your ulcer bandaged or covered with a wound dressing. While you may have heard about “airing out” wounds, experts now know that not covering a wound actually increases infection odds and slows healing[11].
Natural Remedies and Supporting Therapies
Several natural approaches can support conventional treatment:
- Aloe Vera: Known for wonderful healing and rejuvenating effects on skin, aloe vera’s antibacterial properties play a vital role in speeding up diabetic foot ulcer treatment[12].
- Tea Tree Oil: Rich in antibacterial properties, tea tree oil mixed with coconut oil can be used for dressing diabetic foot ulcers[12].
- Flaxseed Oil: These seeds work on vascular damage, a root cause of diabetic foot ulcers. Rich in omega-3 fatty acids, they’re necessary for repairing damaged blood vessels[12].
Advanced Technology in Diabetic Foot Ulcer Management
Cold Plasma Technology Specifications
The integration of cold plasma technology in diabetic foot ulcer treatment represents a significant advancement. The Mirari Cold Plasma system from miraridoctor.com offers precise therapeutic parameters:
| Technical Parameter | Specification |
|---|---|
| Frequency Range | 50-100 kHz |
| Power Output | 5-12W |
| Plasma Generation | Dielectric Barrier Discharge |
| Active Species | Nitric Oxide (NO) and ROS |
| Treatment Duration | 5-15 minutes per session |
| Operating Temperature | Non-thermal (<40°C) |
Clinical Benefits and Applications
| Application Area | Treatment Duration | Reported Outcomes |
|---|---|---|
| Wound Healing | 10-15 minutes | Accelerated tissue regeneration |
| Infection Control | 5-10 minutes | Broad-spectrum antimicrobial action |
| Pain Management | 10-15 minutes | Reduced inflammation and discomfort |
| Tissue Regeneration | 15 minutes | Enhanced collagen synthesis |
Classification and Severity Assessment
Wagner Ulcer Classification System
Healthcare providers use the Wagner Ulcer Classification System to assess ulcer severity on a scale of 0 to 5:
- Grade 0: No open lesions; may have healed lesion
- Grade 1: Superficial ulcer without penetration to deeper layers
- Grade 2: Deeper ulcer, reaching tendon, bone, or joint capsule
- Grade 3: Deeper tissues involved, with abscess, osteomyelitis, or tendonitis
- Grade 4: Gangrene in a portion of forefoot or heel
- Grade 5: Extensive gangrenous involvement of the entire foot[5]
IWGDF/IDSA Classification for Infection
The International Working Group on the Diabetic Foot (IWGDF) and Infectious Diseases Society of America (IDSA) classification helps assess infection severity and guide treatment decisions[13].
Patient-Focused Frequently Asked Questions
How long does it take for a diabetic foot ulcer to heal?
Healing time depends on various factors including wound size and location, pressure on the wound, circulation, blood glucose levels, and wound care. Healing may occur within weeks or require several months[2]. Proper off-loading and blood sugar control are crucial for optimal healing times.
Can diabetic foot ulcers be prevented completely?
While diabetic foot ulcers cannot always be prevented, research shows that their development is largely preventable with proper foot care[2]. Daily foot inspections, proper footwear, blood sugar control, and regular podiatric care significantly reduce ulcer risk.
What should I do if I notice the first signs of a foot ulcer?
Contact your healthcare provider immediately upon noticing any skin discoloration, unusual swelling, or open wounds. Early intervention is crucial – the quicker your wound heals, the lower the risk of infection and complications[11].
Are there any new treatments showing promise for diabetic foot ulcers?
Yes, several innovative treatments are showing promise, including cold plasma therapy, advanced wound dressings, and bioengineered skin substitutes. The Mirari Cold Plasma system represents one such advancement, offering non-thermal healing through controlled plasma application.
How can family members help with diabetic foot ulcer care?
Family members can assist with daily foot inspections, help maintain proper wound care routines, ensure medication compliance, and provide emotional support. They should also be trained to recognize warning signs that require immediate medical attention.
Prevention: The Best Medicine
Daily Foot Care Routine
Prevention remains the most effective approach to diabetic foot ulcers. A comprehensive daily routine should include:
- Daily Inspection: Check feet daily for cuts, blisters, redness, swelling, or nail problems. Use a mirror to check the bottom of feet if necessary.
- Proper Hygiene: Wash feet daily with lukewarm water and mild soap. Dry thoroughly, especially between toes.
- Appropriate Footwear: Wear shoes that fit properly and provide adequate protection. Avoid walking barefoot, even indoors.
- Regular Professional Care: Schedule regular podiatric examinations and maintain optimal blood glucose control.
Risk Factor Management
Managing underlying risk factors is crucial for prevention:
- Maintain HbA1c levels below 7% when possible
- Control blood pressure and cholesterol
- Quit smoking and limit alcohol consumption
- Manage weight through diet and exercise
- Address peripheral arterial disease if present
The integration of advanced technologies like the Mirari Cold Plasma system into comprehensive diabetic foot care represents a promising evolution in treatment options, offering patients new hope for healing and limb preservation.
Understanding what a diabetic foot ulcer is, recognizing its appearance, and knowing how to treat it properly can mean the difference between healing and amputation, even life and death. With proper care, education, and access to advanced treatment modalities, the devastating impact of diabetic foot ulcers can be significantly reduced.
References
- Wang, X., et al. (2022). Diabetic foot ulcers: Classification, risk factors and management. PMC. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9268853/
- University of Michigan Health. (2004). Frequently Asked Questions: Diabetic Foot Ulcers. UofM Health. https://www.uofmhealth.org/health-library/abq2393
- Feetsee. (2025). What Does Foot Ulcer Look Like? Feetsee. https://www.feetsee.com/what-does-foot-ulcer-look-like/
- Mint STL. (2025). How To Spot The Signs Of A Diabetic Ulcer On The Foot. Mint STL. https://www.mintstl.com/how-to-spot-the-signs-of-a-diabetic-ulcer-on-the-foot/
- Healthline. (2024). Diabetic Foot Ulcers: Causes and Treatments. Healthline. https://www.healthline.com/health/diabetes/diabetic-foot-ulcer
- LA Vascular Specialists. (2025). Can You Die From Diabetic Foot Ulcer. LA Vascular Specialists. https://www.lavascularspecialists.com/can-you-die-from-diabetic-foot-ulcer/
- CINTESIS. (2021). Diabetic Foot Ulcer Associated With High Risk of Death. CINTESIS. https://www.cintesis.eu/en/news/diabetic-foot-ulcer-associated-with-high-risk-of-death/
- Alexiadou, K., et al. (2012). Management of Diabetic Foot Ulcers. PMC. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3353098/
- MedlinePlus. (2024). Diabetes – foot ulcers. MedlinePlus Medical Encyclopedia. https://medlineplus.gov/ency/article/001443.htm
- MyHealth Alberta. (2024). Diabetic Foot Ulcer: Care Instructions. MyHealth Alberta. https://myhealth.alberta.ca/Health/aftercare-information/pages/conditions.aspx?hwid=abq2393
- WebMD. (2024). How to Care for Diabetic Ulcers and Sores. WebMD. https://www.webmd.com/diabetes/diabetic-foot-ulcer-care
- Pristyn Care. (2025). Diabetic Foot Ulcer Home Treatment. Pristyn Care. https://www.pristyncare.com/blog/diabetic-foot-ulcer-home-treatment/
- IDSA. (2023). Diabetic Foot Infections. Infectious Diseases Society of America. https://www.idsociety.org/practice-guideline/diabetic-foot-infections/
Related articles
Made in USA