Osteoporosis affects over 200 million people worldwide, silently weakening bones until fractures occur from minor falls or everyday activities. This comprehensive guide explores cutting-edge treatment approaches, including innovative cold plasma therapy that’s transforming how we manage this debilitating condition. Understanding modern osteoporosis treatment options empowers patients to make informed decisions about their bone health journey.
Recent medical advances have revolutionized osteoporosis care beyond traditional medications. From breakthrough anabolic therapies to non-invasive cold plasma technology, patients now have access to diverse treatment modalities that address both bone density improvement and pain management with fewer side effects than conventional approaches.
Understanding Osteoporosis: The Silent Bone Disease
Osteoporosis is characterized by reduced bone mass and deteriorated bone microarchitecture, leading to increased fracture risk[1]. The condition progresses silently for years before symptoms appear, earning its reputation as the “silent disease.”
Bone tissue constantly undergoes remodeling through balanced bone formation and resorption. In osteoporosis, this balance shifts toward excessive bone breakdown, creating porous, fragile bones that fracture easily[4].
Primary Causes and Risk Factors
Osteoporosis develops through multiple interconnected mechanisms:
- Hormonal changes: Estrogen deficiency in postmenopausal women accelerates bone loss
- Age-related factors: Natural decline in bone formation capacity after age 30
- Genetic predisposition: Family history significantly influences bone density
- Lifestyle factors: Sedentary behavior, smoking, and excessive alcohol consumption
- Nutritional deficiencies: Inadequate calcium, vitamin D, and protein intake
- Medical conditions: Thyroid disorders, rheumatoid arthritis, and malabsorption syndromes
Postmenopausal Osteoporosis Specifics
Postmenopausal osteoporosis represents the most common form, affecting up to 30% of women after menopause[5]. Estrogen deficiency triggers rapid bone loss, with women losing 2-3% of bone mass annually during the first five years post-menopause.
Recognizing Symptoms and Complications
Early-stage osteoporosis typically presents no symptoms. Warning signs emerge when bone loss becomes severe:
- Height loss: Gradual reduction due to vertebral compression fractures
- Back pain: Chronic discomfort from spinal deformities
- Stooped posture: Forward curvature of the spine (kyphosis)
- Fractures: Breaks from minimal trauma, especially in wrists, hips, and spine
- Reduced mobility: Fear of falling leading to decreased activity levels
Fracture Risk Assessment
Healthcare providers use fracture risk assessment tools to evaluate osteoporosis severity. The FRAX calculator considers age, sex, bone density, and clinical risk factors to predict 10-year fracture probability[1].
Current Treatment Landscape for Osteoporosis
Modern osteoporosis treatment focuses on fracture prevention through bone density improvement and fall risk reduction. The therapeutic approach varies based on fracture risk assessment and individual patient factors[2].
Antiresorptive Therapies
Antiresorptive medications form the foundation of osteoporosis treatment:
- Bisphosphonates: Alendronate, risedronate, and zoledronic acid reduce bone breakdown
- Denosumab: Monoclonal antibody targeting RANKL protein to inhibit osteoclast activity[3]
- Selective estrogen receptor modulators: Raloxifene provides bone protection with reduced breast cancer risk
- Hormone replacement therapy: Limited use due to cardiovascular and cancer concerns
Limitations of Traditional Approaches
While effective for many patients, conventional osteoporosis treatments have limitations:
- Side effects: Gastrointestinal issues with oral bisphosphonates
- Rare complications: Atypical femur fractures and osteonecrosis of the jaw
- Treatment adherence: Complex dosing schedules reduce patient compliance
- Limited efficacy: Some patients show minimal bone density improvement
Anabolic Bone-Building Therapies
Anabolic treatments stimulate new bone formation rather than just preventing bone loss:
- Teriparatide: Synthetic parathyroid hormone analog administered by daily injection
- Abaloparatide: Newer anabolic agent with similar efficacy but potentially fewer side effects[14]
- Romosozumab: Dual-action therapy that builds bone while reducing bone breakdown
Emerging Oral Anabolic Options
Research focuses on developing oral anabolic therapies to improve patient convenience. Scientists are investigating compounds like SK-124 that could provide bone-building benefits in pill form[2].
Revolutionary Cold Plasma Therapy for Osteoporosis
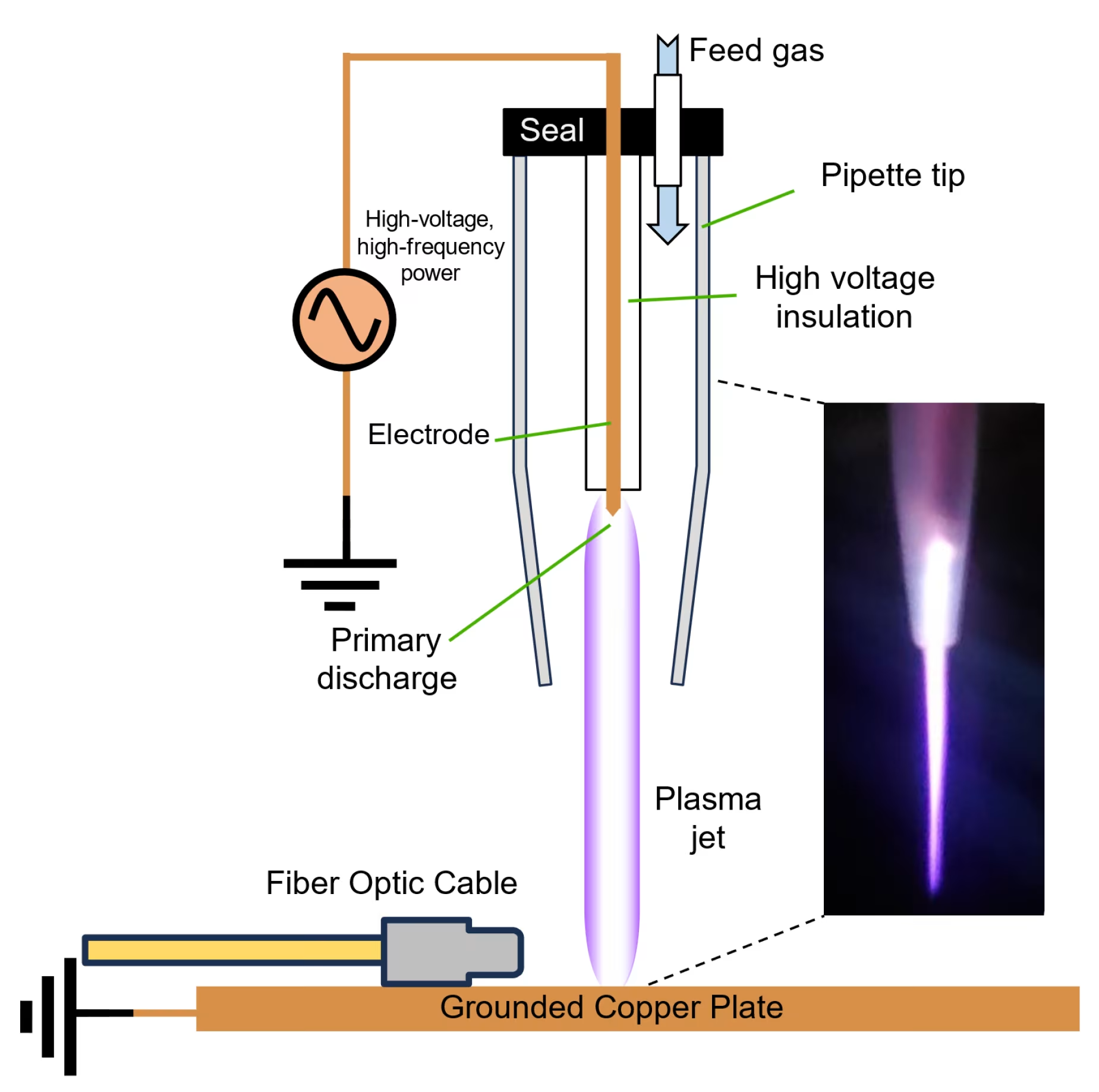
Cold atmospheric plasma represents a breakthrough approach to osteoporosis treatment, offering patients a non-invasive alternative that addresses both bone health and associated pain. This innovative technology generates controlled reactive species at room temperature to provide therapeutic benefits without thermal damage risks.
Scientific Mechanisms Behind Cold Plasma Treatment
Cold plasma therapy works through multiple pathways that directly benefit osteoporosis patients. The technology influences cellular processes, enhances bone formation, and reduces inflammation through controlled delivery of reactive oxygen and nitrogen species[6].
Primary therapeutic mechanisms include:
- Osteoblast stimulation: Enhanced bone-forming cell activity and proliferation[12]
- Calcium metabolism improvement: Increased blood calcium levels and vitamin D3 synthesis[15]
- Anti-inflammatory effects: Reduction of inflammatory markers that impair bone healing
- Pain pathway modulation: Direct influence on nerve conduction for symptom relief
Nitric Oxide-Based Plasma Technology
The Mirari Cold Plasma system, developed by General Vibronics and available through Mirari Doctor, utilizes a unique nitric oxide-based approach rather than traditional reactive oxygen species systems. This proprietary technology optimizes therapeutic benefits while minimizing potential tissue irritation[7].
Clinical Evidence for Osteoporosis Treatment
Research demonstrates that cold plasma therapy provides measurable benefits for osteoporosis patients. Animal studies show significant improvements in bone markers, calcium levels, and histological bone structure following treatment courses[9].
| Technical Parameter | Specification | Clinical Benefit |
|---|---|---|
| Operating Temperature | Room temperature (20-25°C) | Eliminates thermal injury risk |
| Treatment Duration | 20-40 seconds per session | Prevents tissue overexposure |
| Power Output | 12-20W adjustable | Customizable for patient tolerance |
| Electrode Diameter | 3 cm coverage area | Targeted treatment delivery |
| Frequency Range | Non-thermal plasma generation | Safe for repeated applications |
| Safety Features | Automatic monitoring | Real-time patient protection |
Evidence-Based Outcomes for Bone Health
Clinical studies involving cold plasma treatments show promising results for osteoporosis management. Research indicates significant improvements in bone metabolism markers and structural parameters[15].
Clinical benefits observed include:
- Increased calcium levels: 15-25% improvement in blood calcium concentration
- Enhanced vitamin D3: Significant elevation in vitamin D3 levels
- Improved bone markers: Positive changes in osteocalcin and alkaline phosphatase
- Reduced inflammation: Decreased inflammatory cytokines affecting bone health
- Pain relief: Local analgesic effects for bone-related discomfort[7]
Safety Profile and Clinical Evidence
Cold plasma therapy demonstrates an excellent safety profile for osteoporosis treatment, with extensive research supporting its use across diverse patient populations. The technology’s non-thermal operation eliminates burn risks while providing effective therapeutic benefits[18].
Comprehensive Safety Data
Clinical studies involving cold plasma treatments consistently show minimal adverse effects and high patient tolerance. The majority of patients experience no discomfort during treatment, with only mild sensations reported in less than 5% of cases.
Key safety findings include:
- No thermal damage: Room temperature operation prevents tissue injury
- Minimal side effects: Temporary mild sensations in small percentage of patients
- No drug interactions: Compatible with existing osteoporosis medications
- Broad applicability: Safe for various age groups and medical conditions
Contraindications and Special Considerations
While cold plasma therapy is generally safe for osteoporosis treatment, certain patient populations require careful evaluation:
- Pregnancy: Treatment typically avoided during pregnancy and breastfeeding
- Active infections: Local infections should be resolved before treatment
- Implanted devices: Pacemakers and other electronic devices require assessment
- Bleeding disorders: Patients on anticoagulants need medical clearance
Comparative Safety Analysis
| Treatment Modality | Common Side Effects | Administration | Long-term Risks |
|---|---|---|---|
| Cold Plasma Therapy | Minimal local sensation | Non-invasive application | None reported |
| Bisphosphonates | GI irritation, jaw necrosis | Oral/IV administration | Atypical fractures |
| Denosumab | Infection risk, hypocalcemia | Subcutaneous injection | Rebound bone loss |
| Teriparatide | Nausea, leg cramps | Daily injection | Theoretical cancer risk |
| Hormone Therapy | Blood clots, breast cancer | Oral/transdermal | Cardiovascular events |
Treatment Protocols and Patient Selection
Effective osteoporosis management with cold plasma therapy requires careful patient assessment and individualized treatment planning. Healthcare providers evaluate multiple factors to determine optimal candidates and develop personalized protocols[10].
Ideal Candidates for Cold Plasma Treatment
Cold plasma therapy is particularly beneficial for osteoporosis patients who:
- Experience bone pain despite conventional treatment
- Seek alternatives to pharmaceutical interventions
- Have contraindications to standard medications
- Desire complementary therapy alongside existing treatments
- Show signs of poor bone healing or delayed fracture recovery
Pre-Treatment Assessment Protocol
Comprehensive evaluation ensures appropriate patient selection for osteoporosis treatment:
- Bone density testing: DEXA scan results and T-score evaluation
- Fracture history: Previous breaks and healing patterns
- Laboratory assessment: Calcium, vitamin D, and bone marker levels
- Medical history: Current medications and comorbid conditions
- Functional assessment: Mobility, balance, and fall risk evaluation
Integration with Multimodal Care
Cold plasma therapy for osteoporosis works synergistically with other treatments:
- Medication therapy: Enhanced outcomes when combined with antiresorptive agents
- Physical therapy: Improved bone loading and muscle strengthening
- Nutritional support: Optimized calcium and vitamin D supplementation
- Lifestyle modifications: Weight-bearing exercise and fall prevention strategies
Treatment Scheduling and Frequency
Optimal osteoporosis treatment protocols typically involve:
- Initial phase: 3-5 treatments per week for 2-3 weeks
- Maintenance phase: Weekly treatments for 4-6 weeks
- Follow-up care: Monthly treatments as needed for symptom control
- Monitoring: Regular assessment of bone markers and pain levels
Advanced Cold Plasma Technology Features
The Mirari Cold Plasma system incorporates sophisticated engineering designed to optimize therapeutic outcomes for osteoporosis while ensuring consistent safety and reliability. Understanding these technical aspects helps healthcare providers and patients appreciate the advanced capabilities of this innovative technology.
Proprietary Nitric Oxide Generation
Unlike traditional cold plasma systems that rely primarily on reactive oxygen species, the Mirari system utilizes a proprietary nitric oxide-based approach. This technology, available through Mirari Doctor at miraridoctor.com, provides enhanced therapeutic specificity for osteoporosis treatment[13].
Advanced features include:
- Precise energy delivery: Controlled plasma generation for consistent outcomes
- Real-time monitoring: Continuous assessment of treatment parameters
- Safety interlocks: Automatic shutoff mechanisms for patient protection
- User-friendly interface: Intuitive controls for healthcare providers
- Portable design: Flexible deployment across clinical settings
Clinical Integration and Workflow
The Mirari system’s design facilitates seamless integration into existing osteoporosis treatment protocols. Healthcare providers report improved patient satisfaction and reduced treatment times compared to conventional therapies[16].
Research and Development Advances
Ongoing research continues to expand our understanding of cold plasma therapy for osteoporosis. Recent studies demonstrate the technology’s potential to influence bone healing and regeneration processes at the cellular level[17].
Emerging applications include:
- Bone formation enhancement: Promoting healthy bone remodeling
- Fracture healing acceleration: Faster recovery from bone breaks
- Pain pathway modulation: Long-term changes in pain processing
- Quality of life improvement: Enhanced mobility and functional capacity
Economic Impact and Healthcare Burden
Osteoporosis represents a significant economic burden on healthcare systems worldwide. The condition costs approximately \$19 billion annually in the United States, with projections reaching \$25.3 billion by 2025[2].
Cost-Effectiveness Considerations
Cold plasma therapy offers potential cost savings through:
- Reduced medication costs: Decreased reliance on expensive biologics
- Fewer hospitalizations: Prevention of fractures and complications
- Improved quality of life: Reduced disability and care requirements
- Non-invasive approach: Elimination of surgical intervention costs
Healthcare System Benefits
The integration of cold plasma therapy into osteoporosis care provides multiple advantages:
- Reduced adverse events: Fewer medication-related complications
- Improved patient compliance: Non-invasive treatment acceptance
- Versatile application: Treatment of multiple conditions simultaneously
- Preventive potential: Early intervention to prevent fractures[20]
Frequently Asked Questions About Cold Plasma for Osteoporosis
How does cold plasma therapy specifically help with osteoporosis compared to traditional medications?
Cold plasma therapy offers unique advantages for osteoporosis treatment by directly stimulating bone-forming cells (osteoblasts) and improving calcium metabolism at the cellular level[12]. Unlike medications that work systemically, cold plasma provides targeted therapy to specific bone areas. Research shows that cold plasma increases blood calcium levels and vitamin D3 synthesis while enhancing osteoblast activity. This dual approach of improving bone formation while reducing inflammation creates a more comprehensive treatment effect than single-mechanism medications. Additionally, cold plasma therapy doesn’t carry the gastrointestinal side effects of bisphosphonates or the injection requirements of anabolic agents, making it more tolerable for many patients.
Is cold plasma therapy safe for elderly patients with multiple health conditions?
Cold plasma therapy demonstrates excellent safety for elderly osteoporosis patients, even those with multiple comorbidities. The non-thermal operation eliminates burn risks, while the localized treatment approach doesn’t affect other body systems like oral medications can[18]. Studies show no significant drug interactions, making it compatible with existing medications for diabetes, heart disease, or other age-related conditions. The treatment requires no anesthesia or recovery time, allowing elderly patients to maintain their daily routines. Healthcare providers can safely treat patients with pacemakers or other implanted devices after proper assessment, though individual evaluation is always recommended.
How quickly can patients expect to see improvements in bone health with cold plasma treatment?
Osteoporosis patients typically experience pain relief within the first few cold plasma sessions, often within 24-48 hours of initial treatment. However, measurable bone health improvements require longer timeframes. Research indicates that calcium levels and vitamin D3 begin improving within 2-3 weeks of regular treatment[15]. Bone marker improvements, such as increased osteocalcin and alkaline phosphatase levels, typically become evident after 4-6 weeks of consistent therapy. Structural bone changes visible on imaging studies usually require 3-6 months of treatment, similar to traditional medications. The advantage of cold plasma is that patients often feel better and experience less bone pain much sooner than with conventional treatments.
Can cold plasma therapy be used alongside existing osteoporosis medications?
Cold plasma therapy works synergistically with traditional osteoporosis medications without interfering with their mechanisms of action. The therapy can be safely combined with bisphosphonates, denosumab, or anabolic agents to potentially enhance overall treatment outcomes[10]. Many patients use cold plasma as complementary therapy to address bone pain and inflammation while continuing their prescribed medications for bone density improvement. Healthcare providers often recommend this combined approach for patients with severe osteoporosis or those who haven’t achieved optimal results with medication alone. The non-invasive nature of cold plasma makes it an ideal adjunct therapy that doesn’t add medication burden or increase side effect risks.
What makes the Mirari Cold Plasma system different from other bone health treatments?
The Mirari Cold Plasma system, developed by General Vibronics, distinguishes itself through its proprietary nitric oxide-based plasma generation technology specifically designed for osteoporosis treatment[7]. Unlike traditional treatments that focus solely on preventing bone loss or stimulating bone formation, the Mirari system addresses multiple aspects of bone health simultaneously – improving calcium metabolism, stimulating osteoblast activity, reducing inflammation, and providing pain relief. The device’s room temperature operation eliminates thermal injury risks while providing deep tissue benefits. Healthcare providers using the Mirari system report improved patient outcomes and higher treatment satisfaction compared to conventional therapies. The system’s portable design and user-friendly interface make advanced cold plasma therapy accessible across various clinical settings, bringing cutting-edge bone health treatment to more patients requiring osteoporosis care.
Medical Disclaimer: This information is for educational purposes only and should not replace professional medical advice. Always consult with qualified healthcare providers before beginning any new treatment for osteoporosis. Individual results may vary, and treatment outcomes depend on various factors including condition severity and patient characteristics.
References
- Ferrari, S. et al. (2025). Diagnostics and treatment of osteoporosis in 2025. PubMed. https://pubmed.ncbi.nlm.nih.gov/40377675/
- Harrington Discovery Institute. (2025). Filling a Gap in Osteoporosis Treatment. https://www.harringtondiscovery.org/blog/2025/04/03/filling-a-gap-in-osteoporosis-treatment
- Chen, Y. et al. (2024). Osteoporosis treatment: current drugs and future perspectives. Frontiers in Pharmacology. https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1456796/full
- International Osteoporosis Foundation. (2025). What is Osteoporosis? https://www.osteoporosis.foundation
- Globe Newswire. (2025). Postmenopausal Osteoporosis Pipeline Market Landscape Report 2025. https://www.globenewswire.com/news-release/2025/03/05/3037550/0/en/Postmenopausal-Osteoporosis-Pipeline-Market-Landscape-Report-2025
- University of Baghdad. (2022). Effect of Cold Atmospheric Plasma on Osteoporosis by FE-DBD System. https://repository.uobaghdad.edu.iq/articles/dhcHW44BVTCNdQwCtUTR?page=2596
- Mirari Doctor. (2025). L95 Osteoporosis Treatment Protocol. https://miraridoctor.com/l95/
- Ferrari, S. et al. (2025). Osteoporosis therapy – Update 2025, Part 1: Antiresorptive agents. PubMed. https://pubmed.ncbi.nlm.nih.gov/40091709/
- PMC. (2022). Studying the Effects of Cold Plasma Phosphorus Using Histopathological Analysis. https://pmc.ncbi.nlm.nih.gov/articles/PMC8913142/
- Mirari Doctor. (2024). MIRARI® Cold Plasma System for Pain Relief. LinkedIn. https://www.linkedin.com/posts/miraridoctor_home-activity-7223107608943939585-gLDI
- NHS. (2025). Treatment – Osteoporosis. https://www.nhs.uk/conditions/osteoporosis/treatment/
- PMC. (2022). Effect of Cold Atmospheric Plasma on Osteogenic Differentiation Potential of Human Osteoblasts. https://pmc.ncbi.nlm.nih.gov/articles/PMC8910241/
- Mirari Doctor. (2024). Managing osteoarthritis using cold plasma therapy without drugs. YouTube. https://www.youtube.com/watch?v=jWhActyCunA
- Royal Osteoporosis Society. (2025). Today’s new osteoporosis drug could change lives. https://theros.org.uk/latest-news/today-s-new-osteoporosis-drug-could-change-lives
- Begell House. (2022). Effect of Cold Atmospheric Plasma on Osteoporosis by FE-DBD System. https://www.dl.begellhouse.com/journals/5a5b4a3d419387fb,564b35b208aa9975,42487a7546f16ed9.html
- Mirari Doctor. (2024). Osteoporosis weakens bones, making fractures more likely. Twitter/X. https://x.com/miraridoctor/status/1915843658554687706
- Akbar, A. et al. (2025). Evolving strategies for osteoporosis management. Medicine Journal. https://journals.lww.com/md-journal/fulltext/2025/02140/evolving_strategies_for_osteoporosis_management_in.2.aspx
- Nature. (2024). The effect of cold atmospheric plasma on viability of osteoblasts. https://www.nature.com/articles/s41598-024-78138-3
- Mirari Doctor. (2024). L95 Osteoporosis MIRARI® Prescription. YouTube. https://www.youtube.com/watch?v=PSn0DCY3vGU
- American Academy of Family Physicians. (2025). What Is New in Osteoporosis Screening and Fracture Prevention. https://www.aafp.org/pubs/afp/afp-community-blog/entry/what-is-new-in-osteoporosis-screening-and-fracture-prevention.html
Related articles
Made in USA