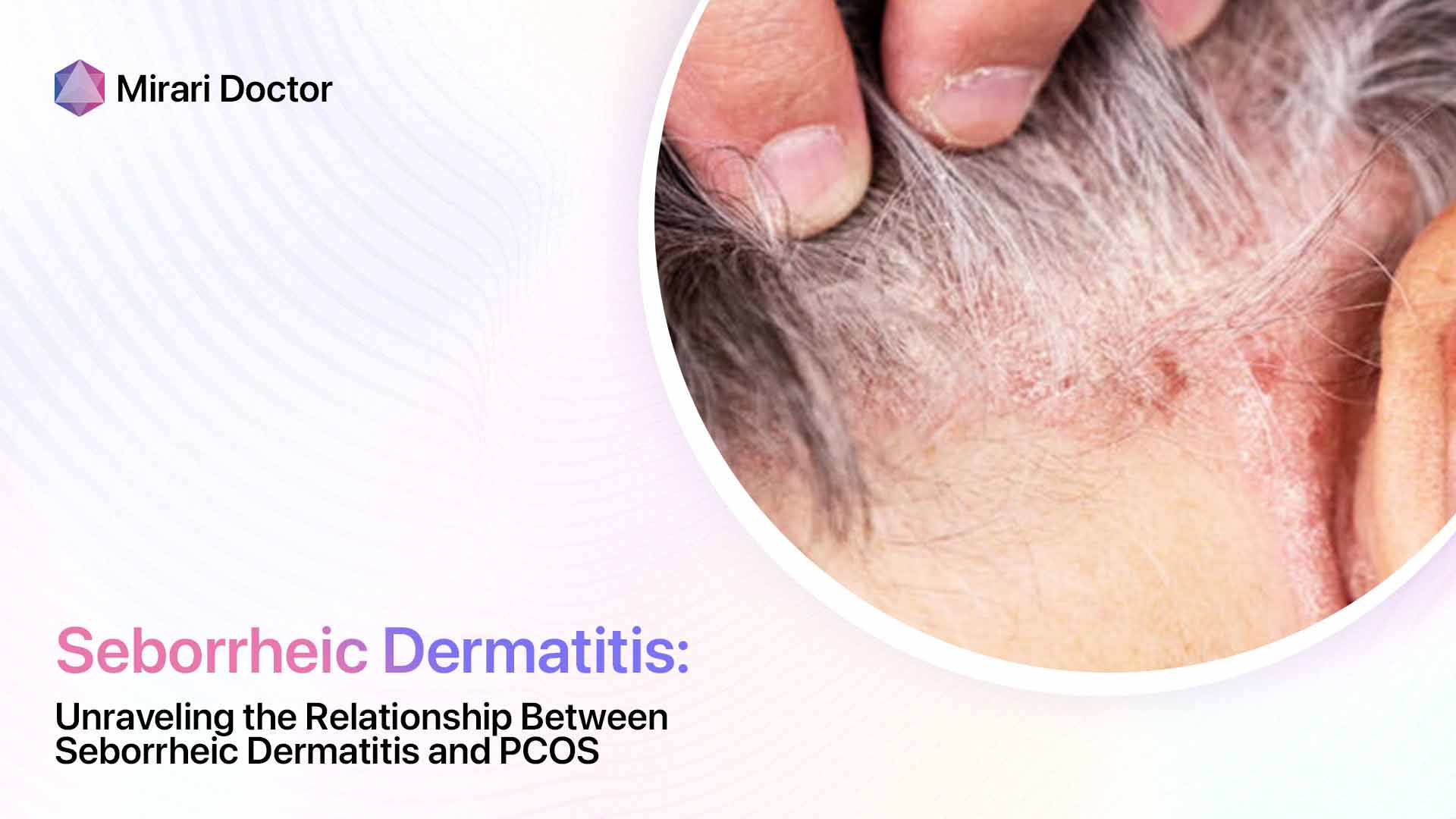
Seborrheic dermatitis is a common inflammatory skin condition that causes red, scaly, itchy rashes, most often on the scalp and face. The exact cause is unknown, but it involves a combination of fungal growth, skin oil secretions, and an overactive immune response. Itraconazole is an oral antifungal medication sometimes used to treat seborrheic dermatitis, especially moderate-severe cases that don’t respond adequately to topical treatments.
Overview of Seborrheic Dermatitis
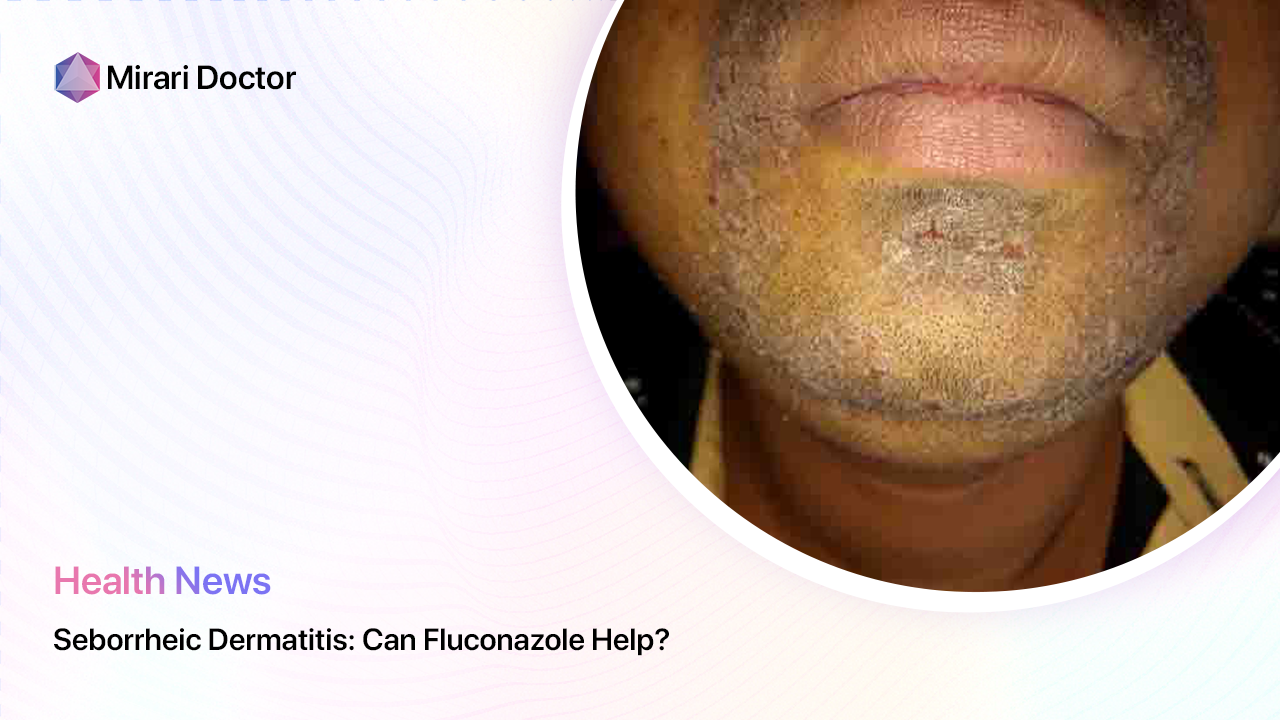
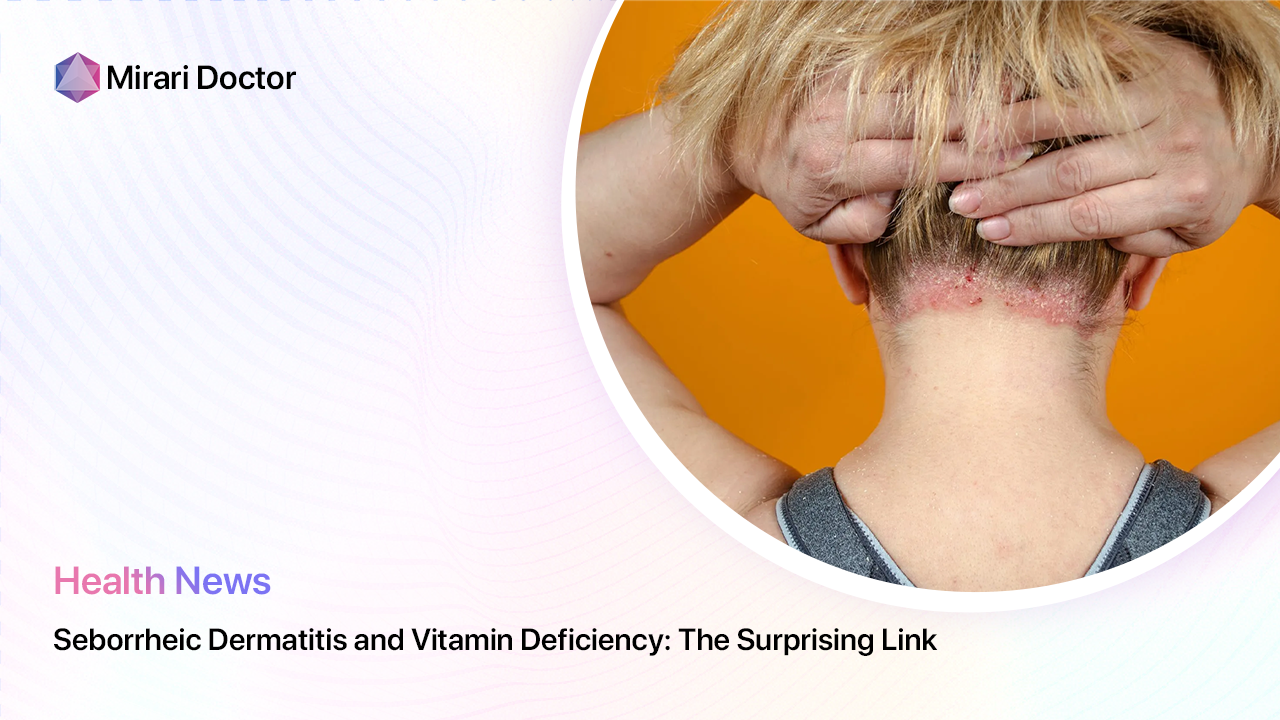
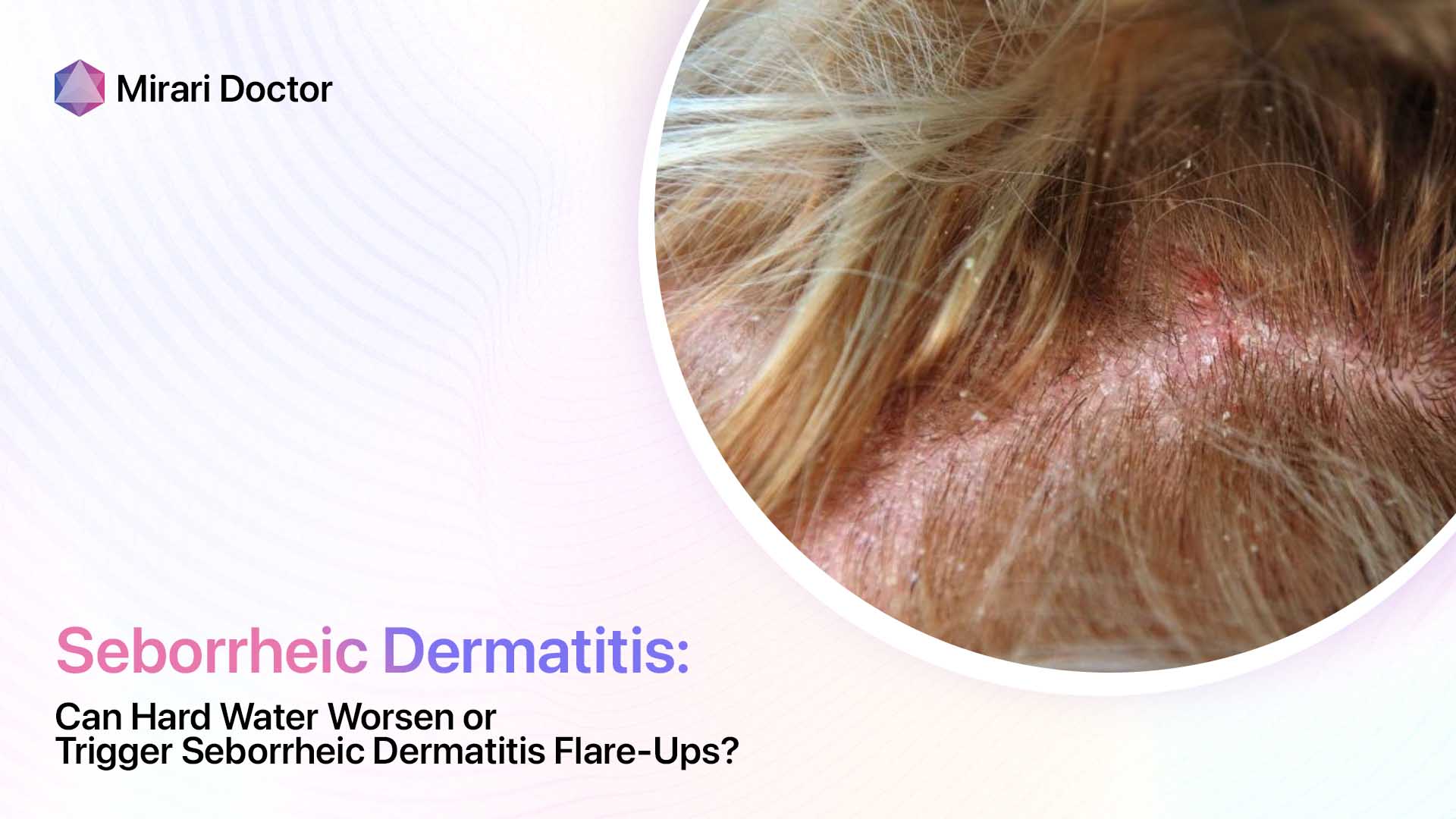
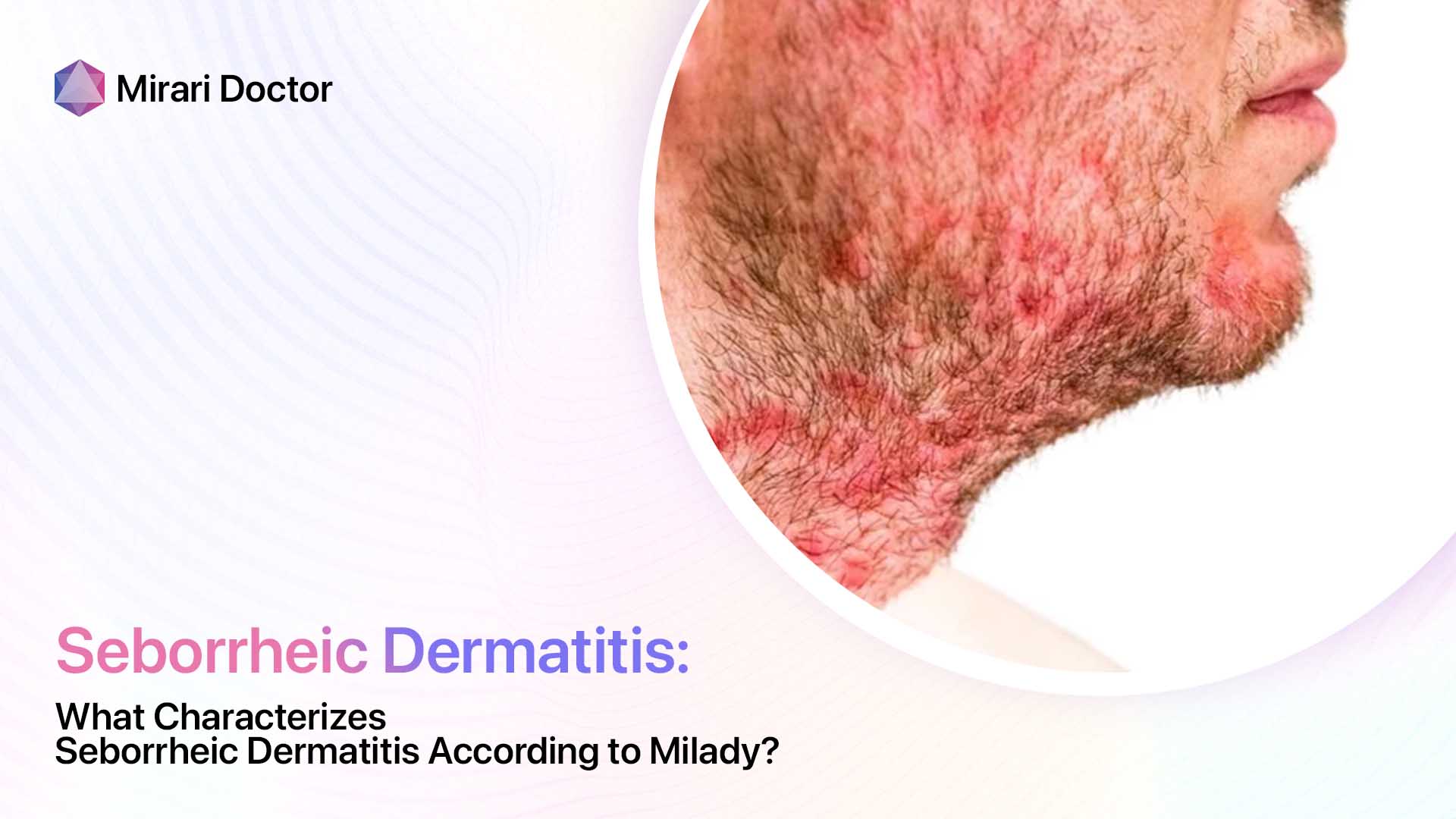
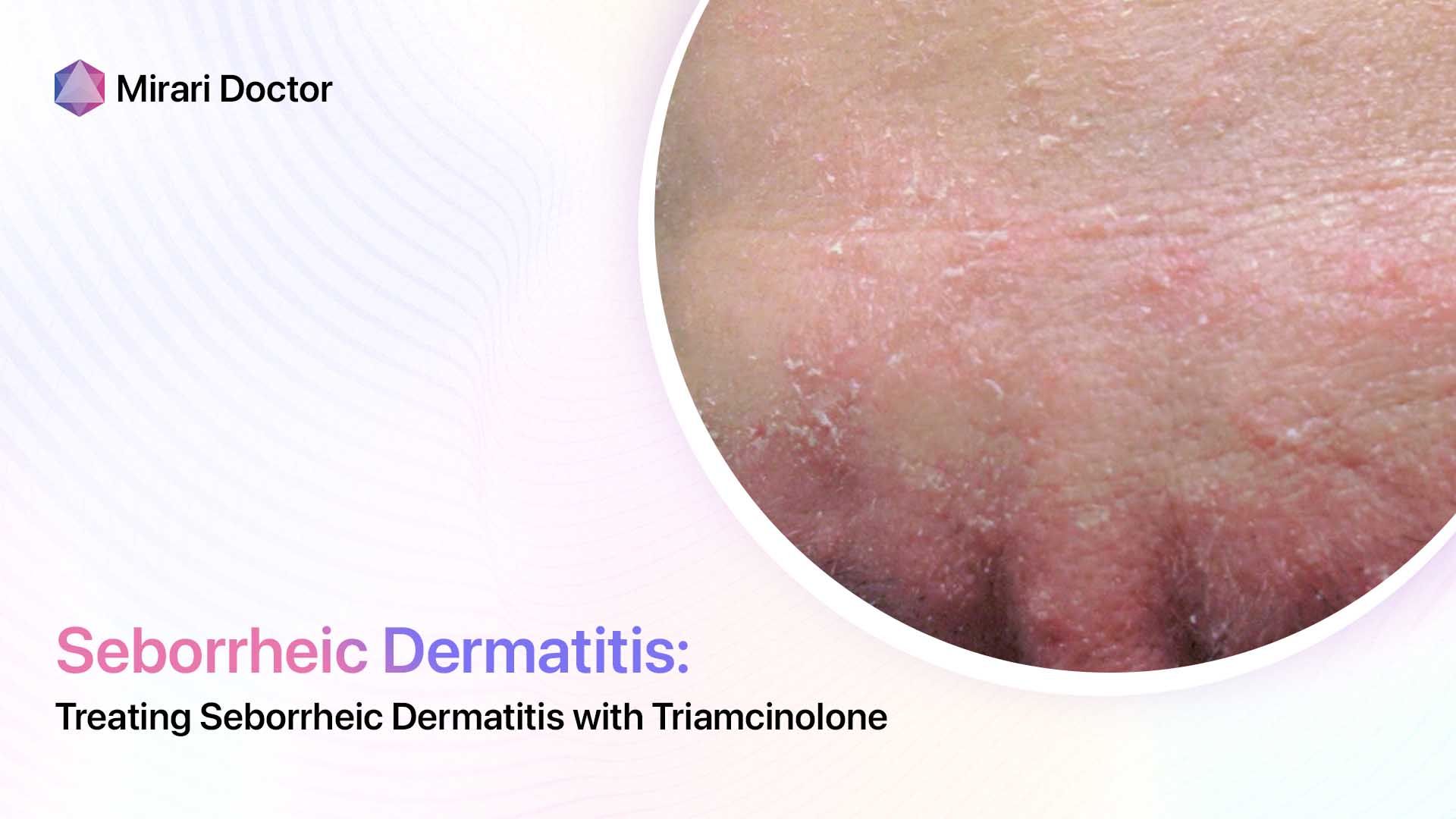
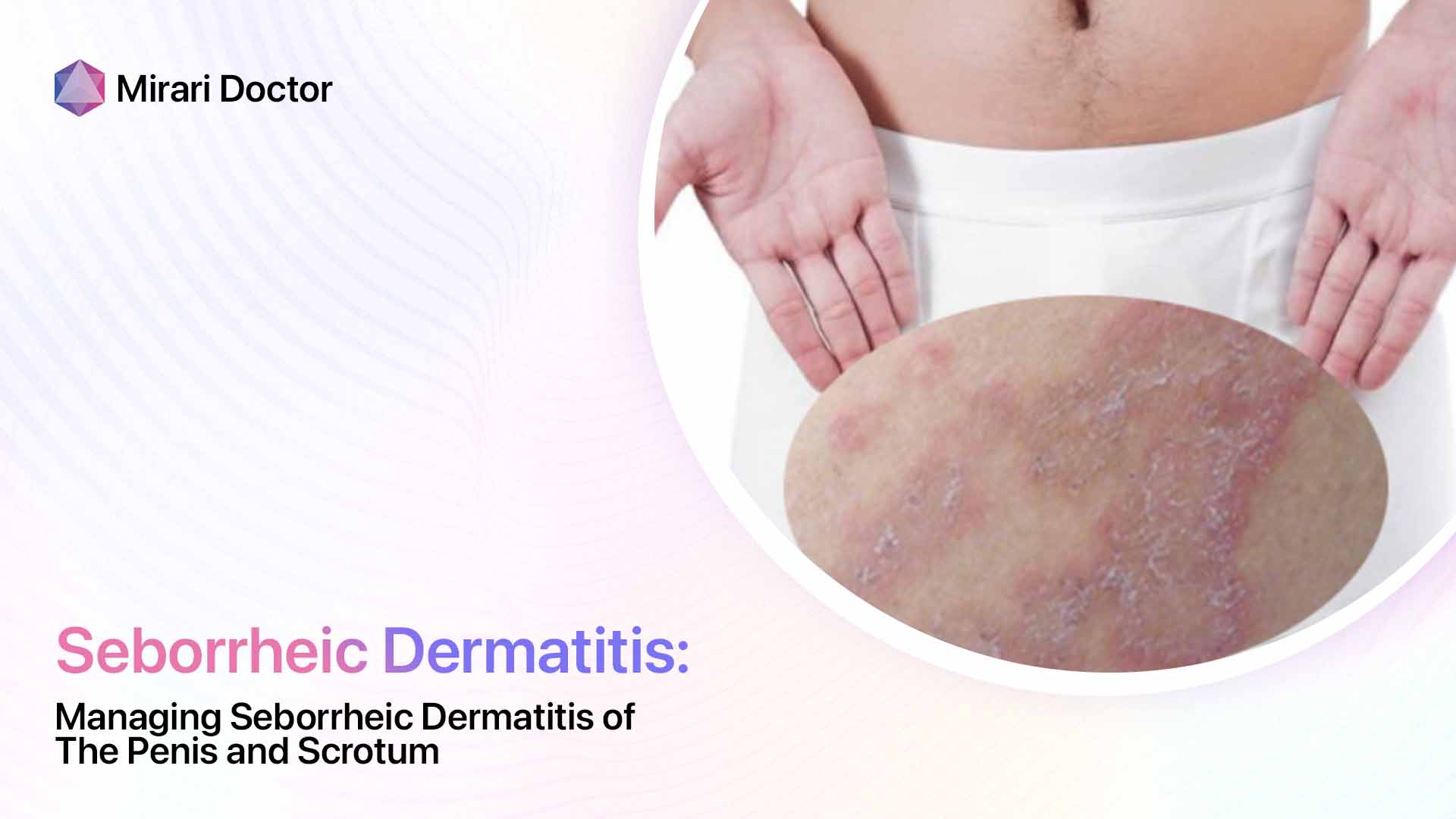
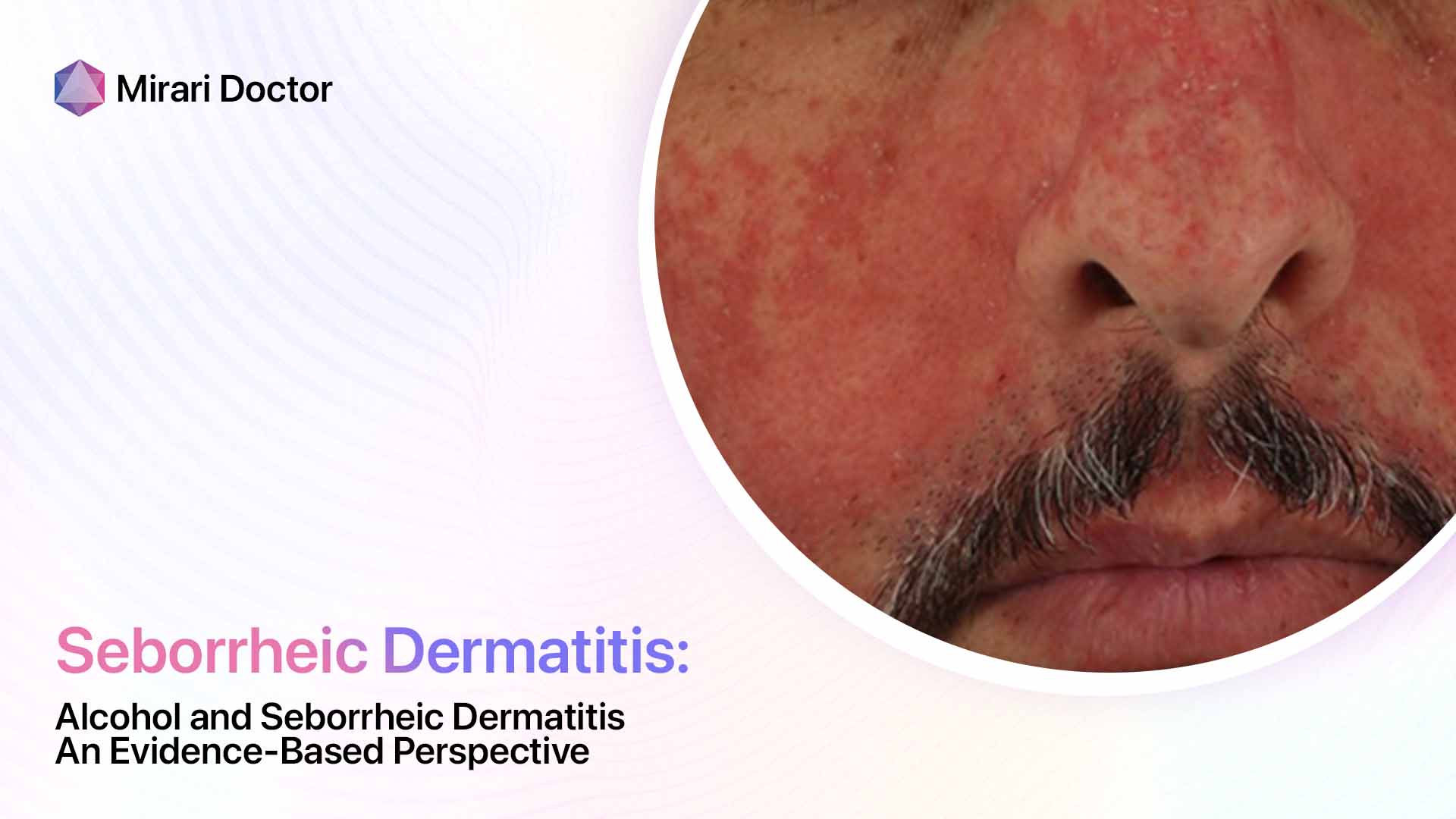
Seborrheic dermatitis causes red, greasy skin covered with flaky white or yellow scales. It most often occurs on the scalp, face (especially eyebrows, sides of the nose, and ears), upper chest, armpits, and groin. Symptoms range from mild dandruff to stubborn, painful rashes spanning large skin areas. Flare-ups may occur sporadically or chronically.
While not dangerous, seborrheic dermatitis significantly reduces one’s quality of life. The unpredictable outbreaks can cause social and workplace distress. Plus the intense itch-scratch cycle leads to further skin inflammation.
Itraconazole is one oral medication sometimes used for seborrheic dermatitis cases not controlled by standard approaches. Let’s explore the evidence behind using itraconazole for seborrheic dermatitis.
What Causes Seborrheic Dermatitis?
Researchers believe seborrheic dermatitis involves an interplay of three primary factors:
- Malassezia – This genus of fungi that naturally lives on everyone’s skin appears to play a major triggering role. While it doesn’t infect or invade the skin, Malassezia releases inflammatory chemicals that seem to spark flare-ups in those with seborrheic dermatitis.
- Skin oils – Excess sebum (oil) production provides a fertile environment for Malassezia to thrive. Oil secretions may also worsen inflammation.
- Immune response – Many experts believe seborrheic dermatitis represents an abnormal inflammatory reaction to Malassezia. The immune system responds aggressively, causing redness, swelling, and flaking.
So in summary, overgrowth of Malassezia yeast plus abundant skin oil allows fungal byproducts to spark an inflammatory immune reaction in those prone to seborrheic dermatitis. Managing outbreaks involves calming inflammation and controlling fungal overgrowth.
Standard Seborrheic Dermatitis Treatment
For mild seborrheic dermatitis, doctors typically first recommend over-the-counter topical antifungal shampoos and creams. These work by reducing fungal overgrowth. First-line topical treatments include:
- Ketoconazole
- Selenium sulfide
- Pyrithione zinc
- Coal tar
If symptoms persist despite a few weeks of topical antifungals, prescription-strength topical steroids like clobetasol may be added to further calm inflammation.
Systemic antifungal medications are generally only used for moderate-severe seborrheic dermatitis unresponsive to topical therapies. Oral itraconazole is one such systemic option.
What is Itraconazole?
Itraconazole is an oral antifungal medication used to treat serious fungal infections. Unlike topical antifungals that only act on the skin’s surface, itraconazole is absorbed into the bloodstream to reach fungi throughout the body.
Besides its antifungal properties, itraconazole also has anti-inflammatory effects that may benefit inflammatory conditions triggered by fungi – like seborrheic dermatitis.
Common U.S. brand names for itraconazole include Sporanox and Onmel.
Evidence for Using Itraconazole in Seborrheic Dermatitis
Several small clinical studies have shown promising results for itraconazole in seborrheic dermatitis treatment.
For example, a 2011 open-label study published in the Indian Journal of Dermatology tested itraconazole in 30 people with stubborn, severe seborrheic dermatitis. Itraconazole dosage was 200 mg per day for four consecutive weeks.
The study found:
- 90% of patients achieved marked disease clearance after one month of itraconazole treatment
- Significant reductions were seen in erythema (redness), scaling, and itching
- Positive effects persisted in most patients six months after stopping itraconazole
The researchers concluded oral itraconazole leads to “remarkable clearance” in severe seborrheic dermatitis “unresponsive to conventional therapy.”
Another trial in 2013 found a similar itraconazole regimen combined with topical tacrolimus maintenance therapy greatly improved severe facial seborrheic dermatitis compared to topical tacrolimus alone.
So evidence indicates short-term oral itraconazole treatment, especially alongside topical anti-inflammatory maintenance, can effectively treat cases of stubborn, severe seborrheic dermatitis.
How Does Itraconazole Help Treat Seborrheic Dermatitis?
Itraconazole is thought to improve seborrheic dermatitis through two key mechanisms:
- Inhibiting fungal overgrowth – Itraconazole is a broad-spectrum antifungal medication. By entering the bloodstream and tissues, it likely reduces Malassezia fungal overgrowth contributing to seborrheic dermatitis flares. Decreasing the overall fungal burden may allow the skin to calm down.
- Anti-inflammatory effects – Beyond just killing fungi, some research shows itraconazole also has immunosuppressive and anti-inflammatory properties. Scientists believe itraconazole may dampen inflammatory pathways that drive seborrheic dermatitis symptoms.
So in summary, itraconazole is thought to improve seborrheic dermatitis both by decreasing fungal overgrowth and mitigating inflammation. For severe cases uncontrolled by topicals targeting one or the other, a systemic oral antifungal/anti-inflammatory like itraconazole may get the condition under control.
Itraconazole Dosage for Seborrheic Dermatitis
Based on available studies, the standard itraconazole dosage regimen for seborrheic dermatitis is:
- 200 mg per day for one week, followed by…
- A second week at 200 mg per day, followed by…
- Maintenance therapy of 200 mg per day for two consecutive days per month.
This cycled approach aims to minimize side effects that can occur with prolonged daily itraconazole use.
Some dermatologists continue maintenance dosing for up to six months. Always follow your prescribing doctor’s specific recommendations.
Potential Itraconazole Side Effects
While often effective, itraconazole does come with potential side effects to consider before starting treatment. Possible adverse effects include:
Common
- Nausea, vomiting, diarrhea
- Headache
- Rash
Rare but serious
- Liver damage
- Heart failure
- Vision changes
- Severe muscle weakness
Due to rare liver toxicity, doctors should monitor liver enzyme levels before and during itraconazole treatment. Individuals with congestive heart failure require very careful monitoring as well.
Itraconazole also interacts with many other medications. Be sure your doctor knows all drugs you currently take before prescribing itraconazole.
Who Shouldn’t Take Itraconazole?
Itraconazole is unsuitable for certain vulnerable groups, including:
- People with liver disease
- Those taking cholesterol-lowering statins
- Individuals dependent on metabolism of certain heart medications
- Pregnant or breastfeeding women
For these higher-risk groups, topical antifungal treatments remain first-line for seborrheic dermatitis. Itraconazole should be avoided.
Lifestyle Measures to Further Control Seborrheic Dermatitis
While medications like itraconazole can effectively treat active seborrheic dermatitis, utilizing lifestyle measures minimizes future flares:
Stress reduction through sufficient sleep, exercise, mindfulness techniques, therapy, etc. Stress strongly triggers seborrheic dermatitis outbreaks for many.
Gentle skin care – avoid harsh soaps, fragrances, oils, and skin products that dry out or irritate skin. Instead, gently cleanse with lukewarm water and mild, fragrance-free cleansers. After cleansing, apply gentle, fragrance-free moisturizers to hydrate and protect skin.
Healthy, balanced nutrition provides skin the nutrients it needs to function optimally. Focus especially on getting plenty of omega-3s, zinc, selenium, antioxidants like vitamin C and E, and probiotics. Consider talking to your doctor or dietician about any nutritional deficiencies. Supplements tailored for skin health may also help.
Combining lifestyle measures, topical treatments, and in difficult cases short-term oral antifungals like itraconazole gives seborrheic dermatitis patients the best chance at lasting remission.
When to See a Dermatologist for Seborrheic Dermatitis
While mild seborrheic dermatitis often responds sufficiently to over-the-counter topical antifungals, some cases require specialized testing and treatment by a dermatologist. Seek professional care if you experience:
- Severe, painful, and extensive rashes covering large skin areas
- Symptoms persisting despite diligent topical therapy for over one month
- Rashes frequently recurring every 1-2 months despite treatment
- Scalp plaques and skin fissures
- Hair loss along with scalp seborrheic dermatitis
A dermatologist can explore whether an oral systemic medication like itraconazole might get your difficult seborrheic dermatitis under better control. We also offer advanced treatment modalities, like targeted phototherapy, unavailable over-the-counter. Getting an accurate diagnosis and starting on effective therapy quickly leads to the best outcomes with this frustrating condition.
Frequently Asked Questions About Itraconazole for Seborrheic Dermatitis
Is itraconazole prescribed for mild cases of seborrheic dermatitis?
No, itraconazole is only used in select cases of moderate-severe seborrheic dermatitis not controlled by standard topical antifungal treatments.
Due to potential side effects, doctors reserve systemic oral itraconazole for more difficult seborrheic dermatitis unresponsive to first and second-line skin creams.
Mild dandruff and minor occasional seborrheic dermatitis flare-ups on small areas often respond well to over-the-counter shampoos and topicals. No need to jump straight to oral medications.
Does itraconazole permanently cure seborrheic dermatitis?
Unfortunately, no – while itraconazole is very effective for some while taking it, seborrheic dermatitis symptoms often return to some degree whenever treatment stops.
Doctors mainly prescribe short itraconazole courses for difficult flares when other options failed. It “resets” the skin to a healthier state so maintenance therapy has a better chance.
But since itraconazole doesn’t cure the underlying seborrheic dermatitis disease process, flare-ups tend to recur over time without continual treatment.
What tests are needed before starting itraconazole?
As itraconazole can rarely cause severe liver injury, doctors monitor liver blood tests closely before and during treatment. Pre-treatment tests include:
- Liver enzyme test (AST/ALT)
- Bilirubin
- Alkaline phosphatase
Doctors also screen for potential medication interactions and medical conditions making itraconazole too risky. Let your provider know all health conditions and supplements/medications you take.
Does itraconazole lower immune system function?
Itraconazole does not typically suppress the immune system in the way strong systemic steroids like prednisone do.
In high doses long-term, some research shows it may slightly affect immune cell function. But short-term low doses used for seborrheic dermatitis have not clearly been linked to increased infections.
Still, let your doctor know if you develop any signs of infection like fever, cough, sore throat or urinary symptoms while on itraconazole. Rarely the drug makes certain fungal infections more likely.
What are signs of liver toxicity from itraconazole?
Seek immediate medical care if you develop any of the following while taking itraconazole:
- Jaundice – yellowing skin/eyes
- Severe abdominal pain
- Bruising easily
- Bleeding excessively
- Dark urine
- Severe nausea/vomiting
- Extreme fatigue
Liver injury is rare but can be life-threatening. Call 911 or have someone drive you to the ER if you experience serious itraconazole side effects.
Conclusion: Key Takeaways
- Itraconazole is an oral systemic antifungal sometimes used to treat moderate-severe seborrheic dermatitis not controlled by topical treatments.
- Research indicates short itraconazole courses can effectively treat stubborn seborrheic dermatitis flare-ups through antifungal and anti-inflammatory properties.
- Potential side effects like liver toxicity require lab monitoring during treatment. Itraconazole also interacts with many medications.
- While not a cure, itraconazole often induces longer remission when combined with topical maintenance therapy and flare prevention lifestyle changes.
- See a dermatologist if over-the-counter approaches fail to control seborrheic dermatitis outbreaks for over one month – advanced therapies like itraconazole may help.
Related articles
Made in USA