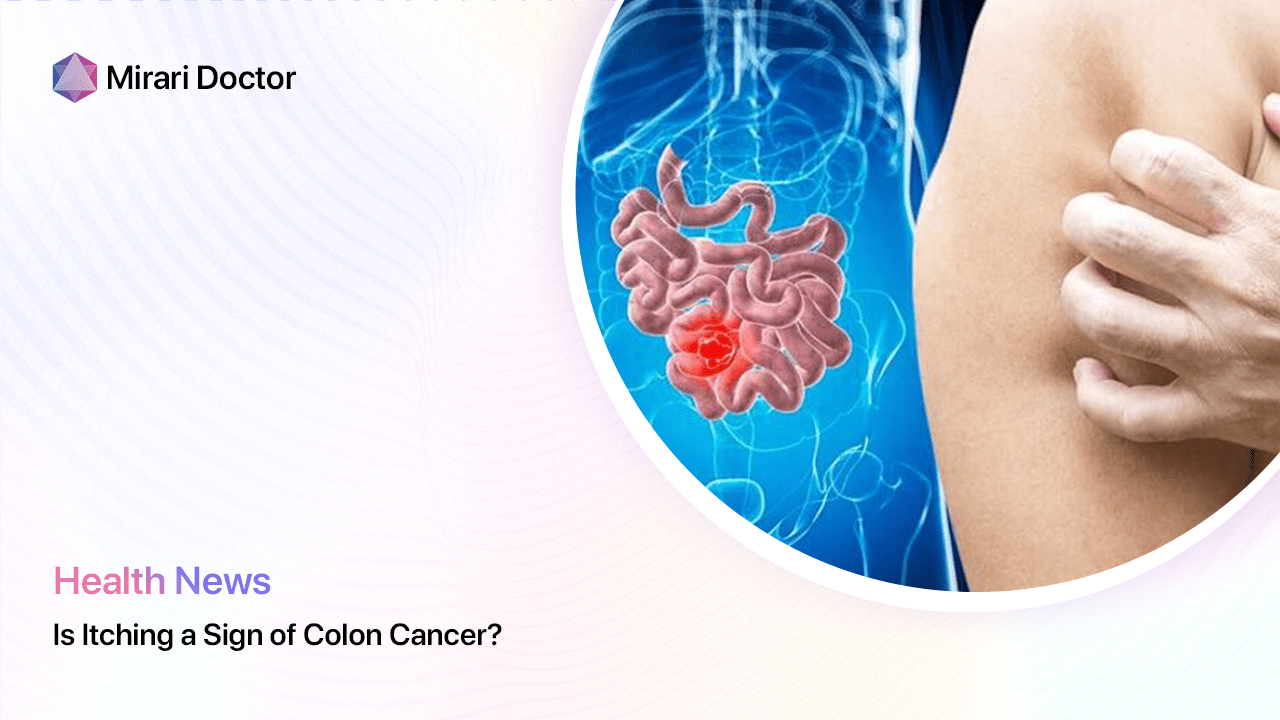
As a medical professional, one of the most common questions I receive from patients is whether certain symptoms, like itching, could be a sign of a serious condition like colon cancer[1]. While itching alone is rarely indicative of colon cancer, it’s important to understand the various symptoms and risk factors associated with this disease. In this article, we’ll explore the potential links between itching and colon cancer, as well as other related conditions and diagnostic methods.
Understanding Colon Cancer
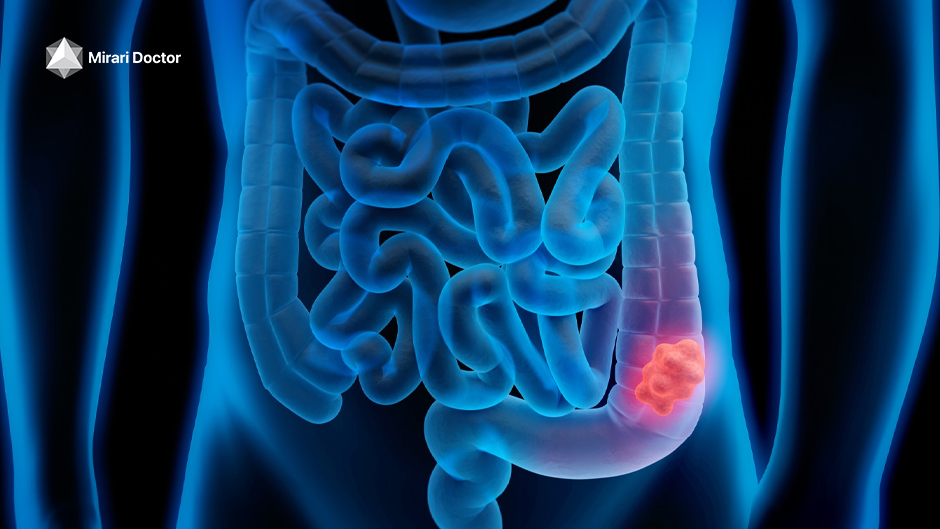
Colon cancer, also known as colorectal cancer, is a type of cancer that begins in the large intestine (colon) or rectum. It typically starts as small, noncancerous (benign) clumps of cells called polyps that form on the inside of the colon. Over time, some of these polyps can become colon cancers[2].
Colon cancer is the third most common cancer diagnosed in both men and women in the United States, excluding skin cancers[3]. The risk of developing colorectal cancer increases with age, with more than 90% of cases occurring in people who are 50 years old or older[4].
Symptoms of Colon Cancer
The symptoms of colon cancer can vary depending on the location and size of the tumor. Some common symptoms include:
- Changes in bowel habits, such as diarrhea, constipation, or narrowing of the stool, that lasts for more than a few days
- A feeling that you need to have a bowel movement that’s not relieved by having one
- Rectal bleeding with bright red blood
- Blood in the stool, which might make the stool look dark brown or black
- Cramping or abdominal pain
- Weakness and fatigue
- Unintended weight loss
It’s important to note that these symptoms can also be caused by other conditions, such as hemorrhoids, inflammatory bowel disease, or infection. However, if you experience any of these symptoms persistently, it’s crucial to consult with a healthcare professional for proper diagnosis and treatment.
Itching as a Symptom of Colon Cancer
While itching, or pruritus, is not a typical symptom of colon cancer, it can be associated with certain complications or related conditions[5]. In some cases, itching may be a sign of a more advanced stage of colon cancer or an indication that the cancer has spread to other parts of the body, such as the liver.
Liver Metastases and Itching
When colon cancer spreads, or metastasizes, it often travels to the liver first. Liver metastases can cause a range of symptoms, including itching, due to the buildup of bile salts in the skin. As the liver becomes compromised by the cancer, it may not be able to effectively process and eliminate bile, leading to a condition called cholestasis[6].
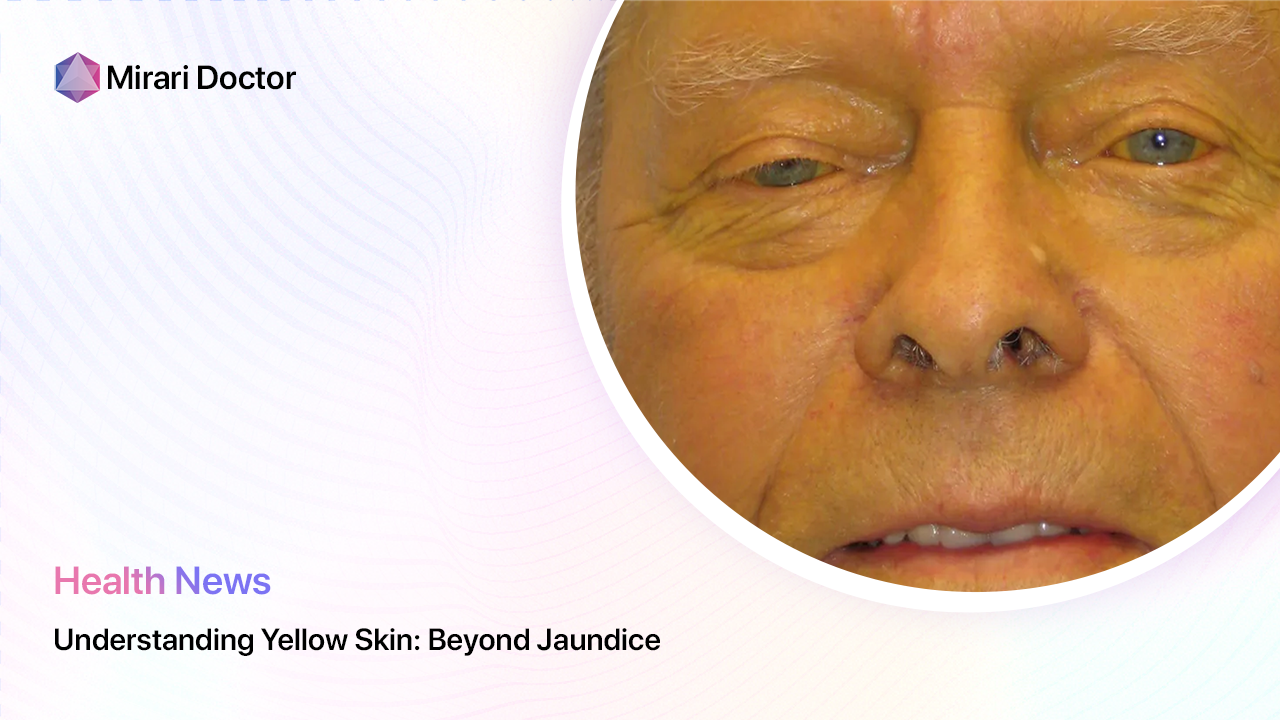
Cholestasis can cause intense itching, typically worse at night, and may be accompanied by other symptoms such as jaundice (yellowing of the skin and eyes), dark urine, and light-colored stools. If you experience these symptoms, it’s essential to inform your healthcare provider promptly.
Paraneoplastic Syndromes and Itching
In some cases, itching associated with colon cancer may be due to paraneoplastic syndromes. These are rare disorders triggered by an abnormal immune system response to a cancerous tumor. Paraneoplastic syndromes can cause a wide range of symptoms, including itching, which may be one of the first signs of an underlying cancer[7].
One example of a paraneoplastic syndrome that can cause itching is Bazex syndrome, also known as acrokeratosis paraneoplastica. This condition is characterized by scaly, psoriasis-like lesions on the hands, feet, ears, and nose, accompanied by severe itching[8]. While Bazex syndrome is more commonly associated with cancers of the upper aerodigestive tract, it has been reported in cases of colon cancer as well.

Other Causes of Itching
It’s crucial to remember that itching can be caused by numerous factors unrelated to colon cancer. Some common causes of itching include:
Skin Conditions
Various skin conditions can cause itching, such as:
- Eczema (atopic dermatitis): A chronic condition that causes dry, itchy, and inflamed skin.
- Psoriasis: An autoimmune disorder that causes the rapid buildup of skin cells, resulting in scaly, itchy patches.
- Dermatitis: Inflammation of the skin caused by contact with irritants or allergens.
Allergic Reactions
Allergic reactions to substances like food, medications, or environmental factors can cause itching, rashes, and hives. Common allergens include:
- Pollen
- Pet dander
- Dust mites
- Certain foods (e.g., nuts, shellfish)
- Latex
Infections
Certain infections, both bacterial and viral, can cause itching. Some examples include:
- Fungal infections: Such as athlete’s foot, jock itch, and ringworm.
- Parasitic infections: Like scabies and lice.
- Sexually transmitted infections (STIs): Such as genital herpes and pubic lice.
Systemic Conditions
In some cases, itching may be a symptom of an underlying systemic condition, such as:
- Liver disease: As mentioned earlier, liver dysfunction can lead to cholestasis and itching.
- Kidney disease: Chronic kidney disease can cause dry, itchy skin due to the buildup of waste products in the body.
- Thyroid disorders: Both hyperthyroidism and hypothyroidism can cause itchy skin.
When to Seek Medical Attention
While itching alone is not typically a cause for concern, there are certain situations in which you should consult a healthcare professional:
- Persistent itching that lasts for more than two weeks
- Itching accompanied by other symptoms, such as weight loss, fatigue, or changes in bowel habits
- Itching that affects your quality of life or disrupts your sleep
- Visible changes in the appearance of your skin, such as rashes, bumps, or discoloration
- Itching that does not respond to over-the-counter treatments or self-care measures
Your healthcare provider can help determine the underlying cause of your itching and recommend appropriate treatment options.
Diagnosing Colon Cancer
If your healthcare provider suspects that your symptoms may be related to colon cancer, they will likely recommend one or more diagnostic tests. These may include:
Colonoscopy
A colonoscopy is the most common and effective method for diagnosing colon cancer. During this procedure, a long, flexible tube equipped with a camera is inserted into the rectum and guided through the entire colon. This allows the doctor to visually inspect the lining of the colon and rectum for any abnormalities, such as polyps or tumors. If necessary, the doctor can also take tissue samples (biopsies) during the procedure for further analysis.
Stool Tests
Stool tests, such as the fecal occult blood test (FOBT) or fecal immunochemical test (FIT), can help detect the presence of blood in the stool, which may be a sign of colon cancer. These tests are often used as a screening tool for individuals at average risk of developing colon cancer[9].
Imaging Tests
In some cases, imaging tests may be used to help diagnose colon cancer or determine the extent of the disease. These may include:
- Computed tomography (CT) scan
- Magnetic resonance imaging (MRI)
- Positron emission tomography (PET) scan
- Ultrasound
Treatment Options for Colon Cancer
If colon cancer is diagnosed, your healthcare provider will work with you to develop an appropriate treatment plan based on the stage and location of the cancer, as well as your overall health and personal preferences. Treatment options may include:
Surgery
Surgery is the most common treatment for colon cancer, especially in the early stages. The goal of surgery is to remove the cancerous tissue and a portion of healthy tissue surrounding it to help prevent the cancer from spreading. The type of surgery performed will depend on the location and size of the tumor, as well as the stage of the cancer[10].
Chemotherapy
Chemotherapy involves the use of drugs to kill cancer cells. It may be recommended before surgery to shrink the tumor (neoadjuvant therapy) or after surgery to help prevent the cancer from returning (adjuvant therapy). Chemotherapy can also be used as a primary treatment for advanced-stage colon cancer that has spread to other parts of the body.
Radiation Therapy
Radiation therapy uses high-energy radiation to kill cancer cells. It is not commonly used for colon cancer, but it may be recommended in certain situations, such as when the cancer has spread to the rectum or if the patient is not a candidate for surgery.
Targeted Therapy
Targeted therapy involves the use of drugs that specifically target the genes, proteins, or tissue environment that contribute to cancer growth and survival. These therapies are designed to block the growth and spread of cancer cells while minimizing damage to healthy cells. Examples of targeted therapies for colon cancer include bevacizumab (Avastin) and cetuximab (Erbitux).

Prognosis and Survival Rates
The prognosis for colon cancer depends on various factors, including the stage of the cancer at the time of diagnosis, the patient’s overall health, and the response to treatment. In general, the earlier colon cancer is detected and treated, the better the outcome.
According to the American Cancer Society, the five-year relative survival rates for colon cancer by stage are[11]:
| Stage | 5-Year Relative Survival Rate |
|---|---|
| I | 92% |
| IIA | 87% |
| IIB | 65% |
| IIC | 53% |
| IIIA | 90% |
| IIIB | 72% |
| IIIC | 53% |
| IV | 12% |
It’s important to remember that these numbers are based on averages and may not necessarily reflect an individual’s unique situation. Additionally, survival rates continue to improve with advancements in screening, early detection, and treatment options.
Prevention and Screening
While not all cases of colon cancer can be prevented, there are steps you can take to reduce your risk:
Lifestyle Changes
- Maintain a healthy weight
- Engage in regular physical activity
- Consume a diet rich in fruits, vegetables, and whole grains
- Limit your intake of red and processed meats
- Avoid excessive alcohol consumption
- Don’t smoke
Screening
Regular colon cancer screening is crucial for early detection and prevention. The American Cancer Society recommends that individuals at average risk of colorectal cancer start regular screening at age 45[12]. Several screening options are available, including:
- Colonoscopy (every 10 years)
- Flexible sigmoidoscopy (every 5 years)
- CT colonography (virtual colonoscopy) (every 5 years)
- Stool-based tests (yearly)
Talk to your healthcare provider about which screening option is best for you based on your age, personal and family medical history, and any symptoms you may be experiencing.
Conclusion
While itching is not a typical symptom of colon cancer, it can be associated with certain complications or related conditions, such as liver metastases or paraneoplastic syndromes. It’s essential to be aware of the various symptoms and risk factors associated with colon cancer and to consult with a healthcare professional if you experience any persistent or concerning symptoms.
Regular colon cancer screening, along with lifestyle modifications, can help reduce your risk of developing this disease and improve your overall health. Remember, early detection and treatment are key to achieving the best possible outcome.
If you have any questions or concerns about your risk for colon cancer or are experiencing symptoms like itching, don’t hesitate to reach out to your healthcare provider. They can provide personalized guidance and support to help you maintain optimal colorectal health.
References
- American Cancer Society. (2021). What Is Colorectal Cancer?
- National Cancer Institute. (2021). Colon Cancer Treatment (PDQ®)–Patient Version.
- American Cancer Society. (2021). Key Statistics for Colorectal Cancer.
- American Cancer Society. (2021). Colorectal Cancer Risk Factors.
- Fazio, V. W., & Church, J. M. (2008). Complications, Causes, Prevention, and Management of Complications in Colorectal Surgery. Surgical Clinics of North America, 88(5), 1089-1103.
- Kremer, A. E., & Oude Elferink, R. P. J. (2014). Cholestatic Pruritus: Pathogenesis and Treatment. Digestive Diseases, 32(5), 637-645.
- Pelosof, L. C., & Gerber, D. E. (2010). Paraneoplastic Syndromes: An Approach to Diagnosis and Treatment. Mayo Clinic Proceedings, 85(9), 838-854.
- Tan, W. P., & Tan, S. H. (2016). Bazex Syndrome and Adenocarcinoma of the Colon. International Journal of Women’s Dermatology, 2(4), 135-136.
- Imperiale, T. F., Ransohoff, D. F., Itzkowitz, S. H., Levin, T. R., Lavin, P., Lidgard, G. P., Ahlquist, D. A., & Berger, B. M. (2014). Multitarget Stool DNA Testing for Colorectal-Cancer Screening. New England Journal of Medicine, 370(14),1287-1297.
- Vogel, J. D., Eskicioglu, C., Weiser, M. R., Feingold, D. L., & Steele, S. R. (2017). The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Treatment of Colon Cancer. Diseases of the Colon & Rectum, 60(10), 999-1017.
- American Cancer Society. (2021). Colorectal Cancer Survival Rates.
- American Cancer Society. (2021). American Cancer Society Guideline for Colorectal Cancer Screening.
Related articles
Made in USA