A staggering 1.9 million Americans are expected to be diagnosed with cancer in 2024, according to the American Cancer Society[1]. While this number is frightening, there is also hope. In recent years, immunotherapy has emerged as a promising new way to treat cancer. Immunotherapy harnesses the power of a person’s own immune system to fight cancer cells.
But immunotherapy can be expensive, leading many cancer patients to wonder: Will my insurance cover it? In particular, does Blue Cross Blue Shield (BCBS), one of the largest health insurance companies in the United States, cover immunotherapy for cancer?
The short answer is: It depends. BCBS coverage of immunotherapy varies based on the specific BCBS plan, the type of cancer, and other factors. However, BCBS does cover many types of immunotherapy for cancer when it is deemed medically necessary.
In this article, we’ll take an in-depth look at what immunotherapy is, how it works to fight cancer, and which types of cancer it is most commonly used for. Then we’ll dive into the specifics of BCBS coverage for immunotherapy, including the requirements that need to be met and the potential out-of-pocket costs. By the end, you’ll have a clearer picture of whether immunotherapy may be a covered option for you or your loved one.
What is Immunotherapy?
Immunotherapy is a type of cancer treatment that boosts the body’s natural defenses to fight cancer. It uses substances made by the body or in a laboratory to improve or restore immune system function[2].
The immune system is a complex network of organs, cells, and molecules that work together to defend the body against invaders, such as bacteria, viruses, and cancer cells. Normally, the immune system can recognize and destroy abnormal cells, including cancer cells.
However, cancer cells have ways to avoid detection and destruction by the immune system. For example, cancer cells can:
- Have genetic changes that make them less visible to the immune system
- Have proteins on their surface that turn off immune cells
- Change the normal cells around the tumor so they interfere with how the immune system responds
Immunotherapy helps the immune system to better recognize and attack cancer cells. There are several types of immunotherapy used to treat cancer, which we’ll discuss next.
How Does Immunotherapy Work for Cancer Treatment?
Immunotherapy works against cancer in two main ways:
- Stimulating, or boosting, the natural defenses of your immune system so it works harder or smarter to find and attack cancer cells.
- Giving your immune system components, such as man-made immune system proteins, to help it do its job better[2].
Some types of immunotherapy are also sometimes called targeted treatments or biological therapies.
The main types of immunotherapy currently being used to treat cancer include:
- Immune checkpoint inhibitors: These drugs block immune system checkpoints that normally keep immune responses in check. This allows immune cells called T cells to more effectively kill cancer cells. Examples include drugs that target the PD-1/PD-L1 and CTLA-4 pathways.
- CAR T-cell therapy: This approach involves collecting a patient’s own immune cells (T cells), genetically modifying them in the lab to attack cancer, and infusing them back into the patient. The T cells are altered to have receptors called chimeric antigen receptors (CARs) on their surface, allowing them to better recognize and attack cancer cells.
- Monoclonal antibodies (mAbs): These are man-made versions of immune system proteins designed to attack a very specific part of a cancer cell. Some mAbs mark cancer cells so that they will be better seen and destroyed by the immune system.
- Cancer vaccines: Vaccines are substances put into the body to start an immune response against certain diseases. Some vaccines are being developed to boost the immune system to better recognize and fight cancer cells.
- Cytokines: Cytokines are proteins that are naturally made by immune system cells. They play important roles in controlling the growth and activity of other immune system cells and blood cells. Man-made versions of cytokines, such as interleukins and interferons, are sometimes used to treat cancer.
The type of immunotherapy a person receives depends on various factors, including the type of cancer, its stage, and the person’s overall health. Immunotherapy can be given alone or in combination with other cancer treatments, such as chemotherapy, radiation, or surgery.
While immunotherapy has led to remarkable results for some cancer patients, it is not effective for everyone. Researchers are still working to understand why immunotherapy works well for some cancers and individuals but not others. Ongoing clinical trials are testing new immunotherapy approaches and exploring ways to make existing immunotherapies more effective.

What Types of Cancer can be Treated with Immunotherapy?
Immunotherapy has been approved to treat many types of cancer, including some of the most common types like lung cancer and melanoma. However, it is not yet as widely used as surgery, chemotherapy, or radiation therapy.
Here is an overview of some of the main types of cancer currently being treated with immunotherapy:
1. Melanoma
Melanoma is a type of skin cancer that develops in the cells that produce the pigment that gives skin its color (melanocytes). Immunotherapy has led to significant advances in the treatment of advanced melanoma over the past decade.
Several immune checkpoint inhibitors have been approved by the U.S. Food and Drug Administration (FDA) to treat melanoma, including pembrolizumab (Keytruda), nivolumab (Opdivo), and ipilimumab (Yervoy). These drugs block proteins on immune cells that normally keep them from attacking other cells in the body, allowing them to better recognize and destroy melanoma cells.
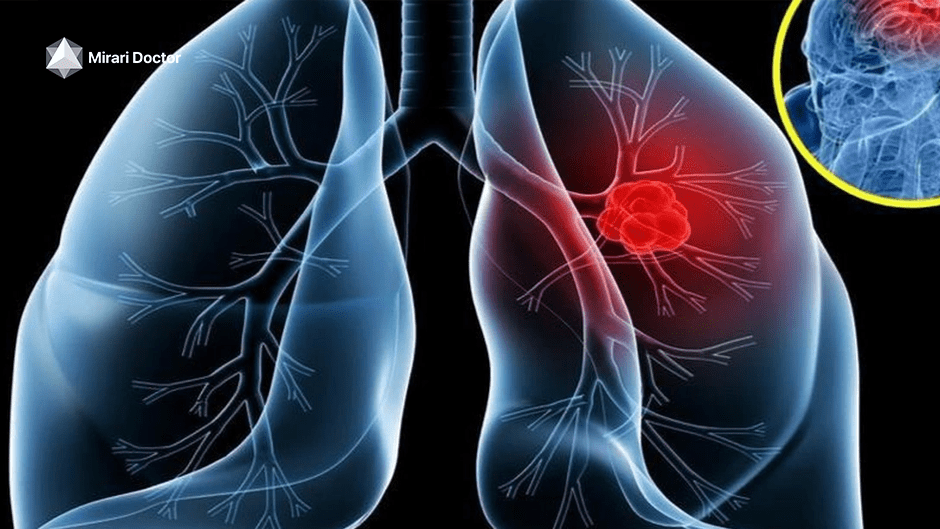
2. Lung Cancer
Lung cancer is the leading cause of cancer death worldwide. Non-small cell lung cancer (NSCLC) is the most common type, accounting for about 85% of all lung cancers[3].
Immune checkpoint inhibitors like pembrolizumab, nivolumab, and atezolizumab (Tecentriq) have become an important treatment option for advanced NSCLC, either alone or in combination with chemotherapy. These drugs work by releasing the brakes on the immune system, allowing it to better recognize and attack lung cancer cells.
3. Kidney Cancer
Kidney cancer, also called renal cancer, is a type of cancer that starts in the kidneys. Renal cell carcinoma (RCC) is the most common type of kidney cancer in adults.
Several immunotherapy drugs have been approved to treat advanced RCC, including immune checkpoint inhibitors like nivolumab and pembrolizumab, as well as cytokines like interleukin-2 (IL-2) and interferon-alfa. These drugs work by stimulating the immune system to better fight kidney cancer cells.
4. Bladder Cancer
Bladder cancer occurs in the tissues of the bladder, the organ in the body that holds and releases urine. Urothelial carcinoma is the most common type of bladder cancer in the United States.
Immunotherapy has become a standard treatment option for some people with advanced bladder cancer. Five different immune checkpoint inhibitors have been approved for bladder cancer: pembrolizumab, nivolumab, atezolizumab, avelumab (Bavencio), and durvalumab (Imfinzi). These drugs work by allowing the immune system to better recognize and attack bladder cancer cells.
5. Leukemia
Leukemias are cancers that start in blood-forming tissue, such as the bone marrow, and cause large numbers of abnormal blood cells to be produced and enter the blood.
One of the most promising immunotherapy approaches for leukemia is CAR T-cell therapy. This involves collecting a patient’s own immune cells, genetically modifying them in the lab to attack leukemia cells, and infusing them back into the patient. Two CAR T-cell therapies, tisagenlecleucel (Kymriah) and brexucabtagene autoleucel (Tecartus), have been approved to treat certain types of leukemia.
While this is not an exhaustive list, it highlights some of the main types of cancer where immunotherapy is making a significant impact. Immunotherapy is also being studied in many other types of cancer, including breast cancer, colorectal cancer, head and neck cancers, liver cancer, and more. As research continues, it is likely that immunotherapy will become an option for a growing number of cancer types.
Is Immunotherapy Covered by Insurance?
1. What is Blue Cross Blue Shield?
Blue Cross Blue Shield (BCBS) is one of the largest health insurance companies in the United States. It is actually a federation of 35 separate United States health insurance companies that provide health insurance in the United States to more than 106 million people.
Despite being made up of many independent companies, BCBS companies all share certain characteristics. They are all licensed by the Blue Cross Blue Shield Association, a trade association that owns the BCBS names and marks. They also all offer certain minimum levels of coverage and participate in the BlueCard program, which allows members to receive coverage when they are away from home.
2. Does Blue Cross Blue Shield Cover Immunotherapy for Cancer?
The answer is that BCBS coverage of immunotherapy for cancer varies depending on the specific BCBS plan and the individual patient’s situation. However, BCBS does cover immunotherapy in many cases when it is deemed medically necessary.
Several BCBS companies have recognized certain hospitals within their networks as Blue Distinction Centers for Cellular Immunotherapy[4]. These are hospitals that have demonstrated expertise in delivering high-quality care for cellular immunotherapy treatments like CAR T-cell therapy for certain cancers.
For example, in 2022, Florida Blue (the BCBS company in Florida) recognized Moffitt Cancer Center with a Blue Distinction Center for Cellular Immunotherapy designation[5]. This means that Florida Blue views Moffitt as a top facility for providing CAR T-cell therapy and other cellular immunotherapies.
However, just because a hospital is a Blue Distinction Center doesn’t necessarily mean all immunotherapy treatments will be covered. Coverage still depends on the specifics of a patient’s BCBS plan.
In general, BCBS plans are more likely to cover immunotherapy when it is:
- FDA-approved for the specific type and stage of cancer
- Prescribed by an in-network provider
- Deemed medically necessary based on the patient’s individual case
Experimental or off-label use of immunotherapy is less likely to be covered.
It’s important for patients to check their specific BCBS plan to understand their coverage. BCBS members can usually do this by logging into their online member portal, calling the customer service number on their insurance card, or talking with their doctor’s office staff.
3. What Types of Immunotherapy are Covered by Blue Cross Blue Shield?
The specific types of immunotherapy covered by BCBS vary based on the individual plan, but may include:
- Immune checkpoint inhibitors like pembrolizumab (Keytruda), nivolumab (Opdivo), and ipilimumab (Yervoy) for cancers like melanoma, lung cancer, and others
- CAR T-cell therapies like tisagenlecleucel (Kymriah) and axicabtagene ciloleucel (Yescarta) for certain types of leukemia and lymphoma
- Monoclonal antibodies like trastuzumab (Herceptin) for HER2-positive breast cancer and rituximab (Rituxan) for certain types of lymphoma and leukemia
- Certain cancer vaccines and cytokines in specific cases
Again, coverage depends on the specific BCBS plan, the patient’s individual medical situation, and other factors like the stage and type of cancer. Patients should verify their coverage with their BCBS plan before starting immunotherapy.
What are the Requirements for Coverage of Immunotherapy by Blue Cross Blue Shield?
There are several key requirements that generally need to be met for BCBS to cover immunotherapy for cancer:
1. Medical Necessity
The immunotherapy treatment must be deemed medically necessary for the individual patient. This means it must be an appropriate treatment option based on factors like:
- The type and stage of cancer
- The patient’s overall health status
- Whether other treatments have been tried first
- Scientific evidence supporting the use of the specific immunotherapy for the patient’s situation
Usually, the patient’s doctor must document the medical necessity and communicate this to BCBS.
2. Pre-authorization
Many BCBS plans require pre-authorization, sometimes called precertification or prior approval, for immunotherapy treatments. This means that the patient’s doctor must submit a request to BCBS explaining the proposed treatment plan and why it is medically necessary before starting treatment.
BCBS will then review the request and decide whether to approve coverage. If pre-authorization is required and not obtained, BCBS may deny coverage.
The pre-authorization process can take some time, so it’s important for patients and doctors to start the process as early as possible.
3. In-Network Providers
As with most health insurance, BCBS generally provides better coverage for services from in-network providers. These are doctors and hospitals that have contracted with BCBS to provide services to members at a discounted rate.
For immunotherapy, patients will likely need to receive treatment from an in-network provider for it to be covered by BCBS. Out-of-network providers may not be covered at all, or may only be covered at a much lower rate, leaving the patient responsible for a larger share of the cost.
The Blue Distinction Centers for Cellular Immunotherapy discussed earlier are an example of in-network providers that are recognized by BCBS for their expertise in delivering immunotherapy treatments.
Patients should work with their doctor and BCBS to ensure they are receiving treatment from an in-network provider whenever possible.
What are the Potential Costs of Immunotherapy with Blue Cross Blue Shield Coverage?
Even with BCBS coverage, patients receiving immunotherapy for cancer may still be responsible for certain out-of-pocket costs. These can include:
1. Deductibles
A deductible is the amount a patient must pay for covered health care services before insurance starts to pay. For example, with a $2,000 deductible, the patient must pay the first $2,000 of covered services themselves.
Deductibles can vary widely across BCBS plans. Some plans have no deductible, while others may have deductibles of several thousand dollars.
2. Co-pays
A co-pay is a fixed amount a patient pays for a covered health care service, usually when they receive the service. For example, a plan might charge a $30 co-pay for each doctor’s visit.
Co-pays for immunotherapy treatments can vary based on the specific BCBS plan. Some plans may have no co-pay, while others could charge a co-pay of $100 or more per treatment.
3. Co-insurance
Co-insurance is a percentage of the total cost of a covered health care service that the patient is responsible for paying. For example, if a plan has 20% co-insurance and an immunotherapy treatment costs $10,000, the patient would be responsible for paying $2,000.
Like deductibles and co-pays, co-insurance amounts can vary significantly across BCBS plans. Some plans may have no co-insurance, while others could have co-insurance of 20%, 30%, or even higher.
It’s important to note that deductibles, co-pays, and co-insurance all contribute to a patient’s overall out-of-pocket costs for immunotherapy. Even with BCBS coverage, these costs can add up quickly, especially for patients requiring multiple immunotherapy treatments over an extended period.
However, many BCBS plans have an out-of-pocket maximum, which is the most a patient will have to pay for covered services in a year. Once this maximum is reached, BCBS will pay 100% of the allowed amount for covered services for the rest of the year.
Patients should carefully review their specific BCBS plan to understand their potential out-of-pocket costs for immunotherapy. They should also talk with their doctor and BCBS about any financial assistance programs or payment plans that may be available to help manage these costs.
FAQs
Is cancer immunotherapy covered by insurance?
Coverage of cancer immunotherapy varies by insurance plan. Many insurance companies, including Blue Cross Blue Shield, do cover immunotherapy when it is deemed medically necessary. However, coverage can depend on factors like the specific type of immunotherapy, the type and stage of cancer, and whether the treatment is FDA-approved for that specific use.
How much does immunotherapy for cancer cost in the US?
The cost of cancer immunotherapy in the United States can be substantial. For example, a single CAR T-cell therapy treatment can cost hundreds of thousands of dollars. Other immunotherapy treatments like immune checkpoint inhibitors can cost tens of thousands of dollars per month. However, the exact cost to the patient will depend on their specific insurance coverage, including factors like deductibles, co-pays, and co-insurance.
What is the cost of immunotherapy for cancer patients?
The out-of-pocket cost of immunotherapy for cancer patients can vary widely based on their insurance coverage. Patients with good insurance may have most of the cost covered, with only small co-pays or co-insurance amounts. However, patients with less comprehensive insurance or no insurance may face very high out-of-pocket costs. It’s important for patients to discuss the potential costs with their doctor and insurance company before starting immunotherapy.
Can immunotherapy cure stage 4 cancer?
While immunotherapy has led to remarkable results for some patients with advanced cancers, including stage 4 cancers, it is not a guaranteed cure. The effectiveness of immunotherapy can vary significantly from person to person and depends on factors like the specific type of cancer, the overall health of the patient, and how well their immune system responds to the treatment. In some cases, immunotherapy may lead to long-term remission or even a cure, but this is not the case for all patients.
What is life expectancy after immunotherapy?
Life expectancy after immunotherapy varies widely depending on the individual patient and their specific cancer. In some cases, immunotherapy has led to long-term survival or even a cure. For example, some patients with advanced melanoma treated with immune checkpoint inhibitors have lived for many years after treatment. However, for other patients, immunotherapy may only provide a temporary benefit or may not be effective at all. Patients should discuss their individual prognosis with their oncologist.
Which cancers respond best to immunotherapy?
Some of the cancers that have shown the best responses to immunotherapy include:
- Melanoma
- Non-small cell lung cancer
- Kidney cancer
- Bladder cancer
- Hodgkin lymphoma
- Head and neck cancers
However, immunotherapy is being studied in many other types of cancer, and new approvals are happening regularly. Even within these types of cancer, individual responses to immunotherapy can vary significantly. Researchers are still working to understand why some cancers and individuals respond better to immunotherapy than others.
Takeaways
- Immunotherapy is a type of cancer treatment that boosts the body’s natural defenses to fight cancer.
- Blue Cross Blue Shield (BCBS) does cover immunotherapy for cancer in many cases when it is deemed medically necessary, but coverage varies based on the specific BCBS plan and the individual patient’s situation.
- BCBS is more likely to cover immunotherapy when it is FDA-approved for the specific type and stage of cancer, prescribed by an in-network provider, and supported by scientific evidence.
- Requirements for BCBS coverage of immunotherapy often include demonstrating medical necessity, obtaining pre-authorization, and using in-network providers.
- Even with BCBS coverage, patients may be responsible for out-of-pocket costs like deductibles, co-pays, and co-insurance. These costs can be substantial, so it’s important for patients to understand their specific plan.
- Immunotherapy has led to significant advances in treatment for cancers like melanoma, lung cancer, kidney cancer, bladder cancer, and leukemia, but it is not effective for all patients.
- Patients considering immunotherapy should discuss the potential benefits, risks, and costs with their oncologist and insurance company to make an informed decision.
References
- American Cancer Society. (2023). Cancer Facts & Figures 2023. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2023/2023-cancer-facts-and-figures.pdf
- National Cancer Institute. (2023). Immunotherapy to Treat Cancer. https://www.cancer.gov/about-cancer/treatment/types/immunotherapy
- American Cancer Society. (2023). Key Statistics for Lung Cancer. https://www.cancer.org/cancer/lung-cancer/about/key-statistics.html
- Blue Cross Blue Shield Association. (2023). Blue Distinction Centers for Cellular Immunotherapy. https://www.bcbs.com/blue-distinction-center/facility/cellular-immunotherapy
- Florida Blue. (2022). Moffitt Cancer Center Recognized as Blue Distinction Center for Cellular Immunotherapy. https://www.floridablue.com/newsroom/moffitt-cancer-center-recognized-blue-distinction-center-cellular-immunotherapy
Related articles
Made in USA