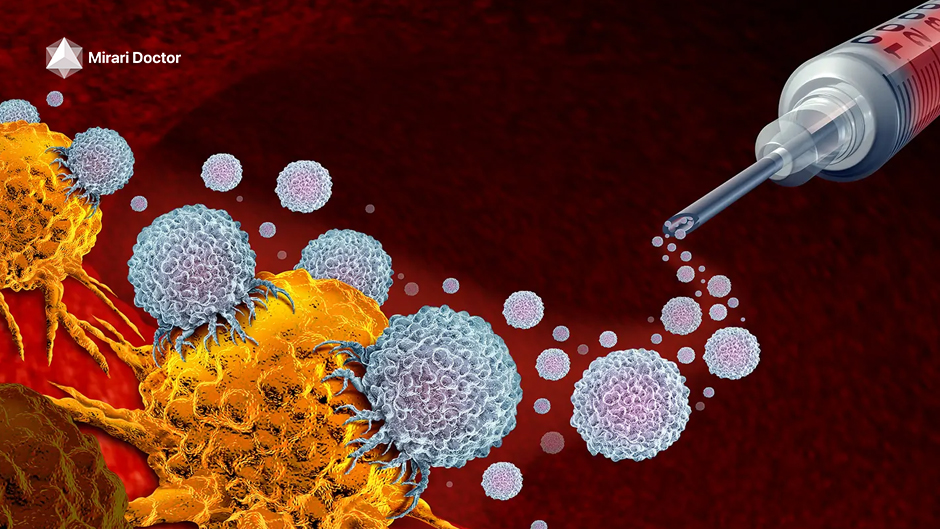
Immunotherapy has transformed the cancer treatment landscape by harnessing the body’s natural defenses to attack malignant cells. From checkpoint inhibitors to CAR T-cell therapy and beyond, these innovative approaches empower the immune system to recognize and eliminate tumors with precision.
However, questions often arise regarding the practical aspects of receiving immunotherapy. Do I need a special device like a port for intravenous (IV) access? How long do the sessions last? Gaining insight equips patients to make informed decisions about their care.
Understanding Immunotherapy Delivery
Traditional Intravenous (IV) Access
Immunotherapy is commonly administered via infusion into a vein. This intravenous route allows the medication to enter the bloodstream and reach cancer cells around the body. The healthcare team inserts a small catheter into a vein, often in the hand or arm, to deliver each infusion session.
The Role of Ports
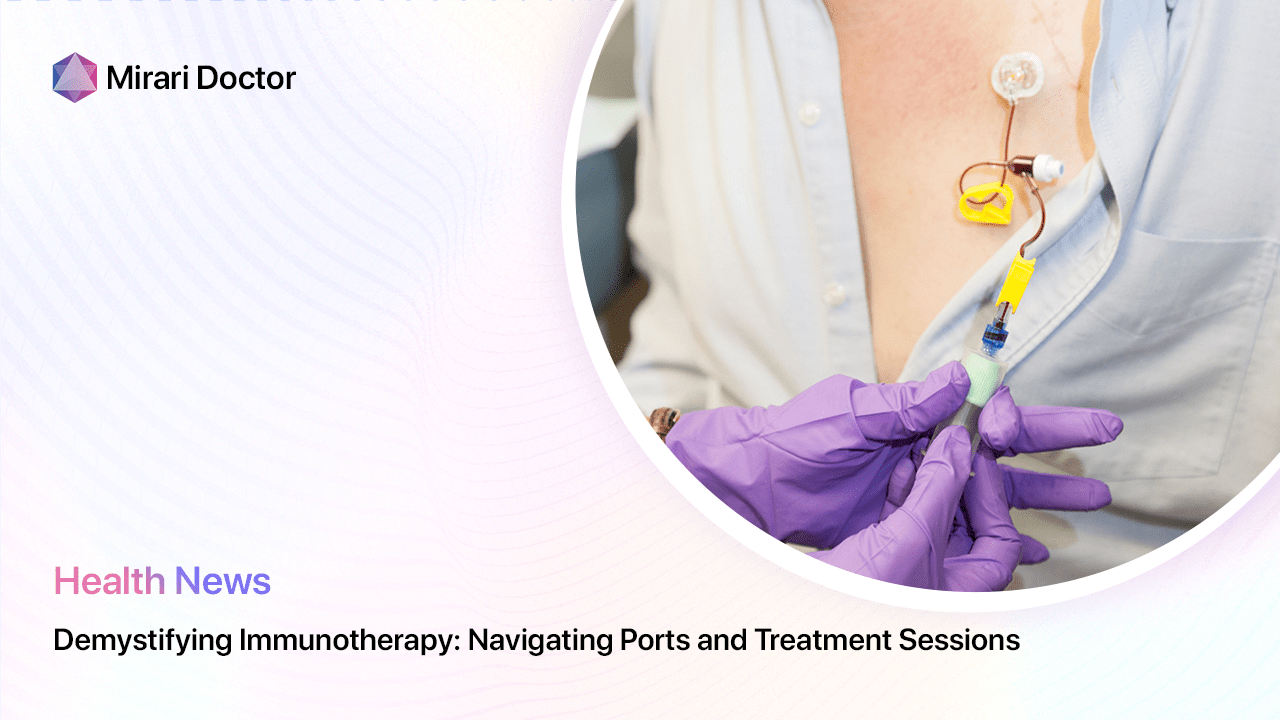
Ports are implantable access devices used for delivering IV therapy, including immunotherapy for cancer. A port consists of a small reservoir with a thin catheter leading to a large vein, typically in the chest. It lies entirely underneath the skin for long-term access.
Ports spare patients from repeated needle sticks for infusions or blood draws. The skin covering the port is numbed before each use, then a special needle pierces through to access the catheter. This convenience makes ports vital for frequent or continuous treatment.
Determining the Need for a Port
Factors to Consider
Variables influencing the decision to get a port include:
- Frequency and overall duration of immunotherapy
- Combination with chemotherapy or other IV therapy
- Difficulty accessing veins for standard IV access
- Patient lifestyle factors and preferences
These aid personalized evaluation of risks, benefits and alternatives like PICC lines. Discussion with your cancer care team is advised.
Benefits and Potential Drawbacks
Ports ease immunotherapy delivery and monitoring, especially for long treatment courses. However, any implanted device carries infection risks needing prompt attention to prevent dangerous complications. Working closely with your medical team ensures optimal safety.
Immunotherapy Treatment Sessions: What to Expect
Session Duration
The length of individual immunotherapy sessions varies widely. Simple IV push methods may take only a few minutes. However, most infusions require 30 minutes up to several hours depending on factors like:
- Volume of medication solution
- Infusion rate based on product guidelines
- Pre- and post-hydration protocols
- Patient tolerance and comfort
Your medical team tailors each session to your situation for maximal security and efficiency.
The Treatment Process
While exact details depend on individual care plans, immunotherapy sessions generally involve:
- Initial check-up of current health status
- IV access placement, often using an existing port if present
- Preconditioning medications as needed
- Slow administration of immunotherapy solution
- Observation period to monitor for reactions
- Post-hydration or medications as necessary
Sessions may incorporate lab tests or scans to track treatment progress as directed by medical protocols or emergence of side effects. Communicating any discomfort or questions that arise during the process helps optimize care.
“Ports can markedly improve quality of life for patients facing repeated treatments and bloodwork.” – Dr. Matthews, surgical oncologist
“While intimidating at first, immunotherapy sessions tend to establish a reassuring routine with time.” – Nurse Gomez
Takeaways
- The use of ports depends on the frequency and duration of immunotherapy, along with patient/clinician preferences.
- Session length varies based on the medication, infusion rate/volume and supplemental protocols.
- Understanding general procedural expectations for immunotherapy appointments enables mental preparation.
- Communicating openly with your cancer care team allows tailoring each element to your needs.
- Demystifying practical aspects helps patients feel empowered in managing immunotherapy.
FAQs
Does everyone receiving immunotherapy need a port?
No, ports are only necessary for regimens requiring very frequent venous access that would be overly painful or difficult with standard IV catheters. However, they greatly facilitate centralized infusions.
What are the benefits of using a port for immunotherapy?
Ports spare patients repeated needle sticks to access veins. They allow rapid, painless medication delivery and blood draws. This makes frequent lab monitoring and long-term treatment safer and more bearable.
Are there any risks associated with using a port?
Any implanted device carries a small infection risk. Signs like pain or fever should prompt immediate consultation, as serious complications can arise if not treated promptly. Overall however, ports often improve quality of life.
How long do immunotherapy sessions typically last?
Session length is highly variable based on the specific medication, treatment regimen/schedule and additional hydration or medication protocols – ranging from less than 30 minutes to several hours.
What should I expect during an immunotherapy session?
Typical procedures include a health checkup, venous access via IV catheter or port, immunotherapy solution administration, monitoring/hydration and post-care as needed. Talk to your doctor regarding your personalized treatment plan.
Related articles
Made in USA