Cold plasma for pressure ulcers represents a groundbreaking advancement in wound care technology, offering new hope for patients struggling with these challenging wounds. This innovative therapy harnesses the power of ionized gas at room temperature to accelerate healing, reduce infection, and improve patient outcomes without the risks associated with traditional thermal treatments.
Pressure ulcers, also known as bedsores or decubitus ulcers, affect millions of patients worldwide and pose significant challenges for healthcare providers. Cold atmospheric plasma (CAP) technology has emerged as a promising solution that addresses multiple aspects of wound healing simultaneously through antimicrobial effects, cellular stimulation, and tissue regeneration.
Understanding Cold Plasma Technology for Pressure Ulcers
Scientific Mechanisms Behind Cold Plasma Healing
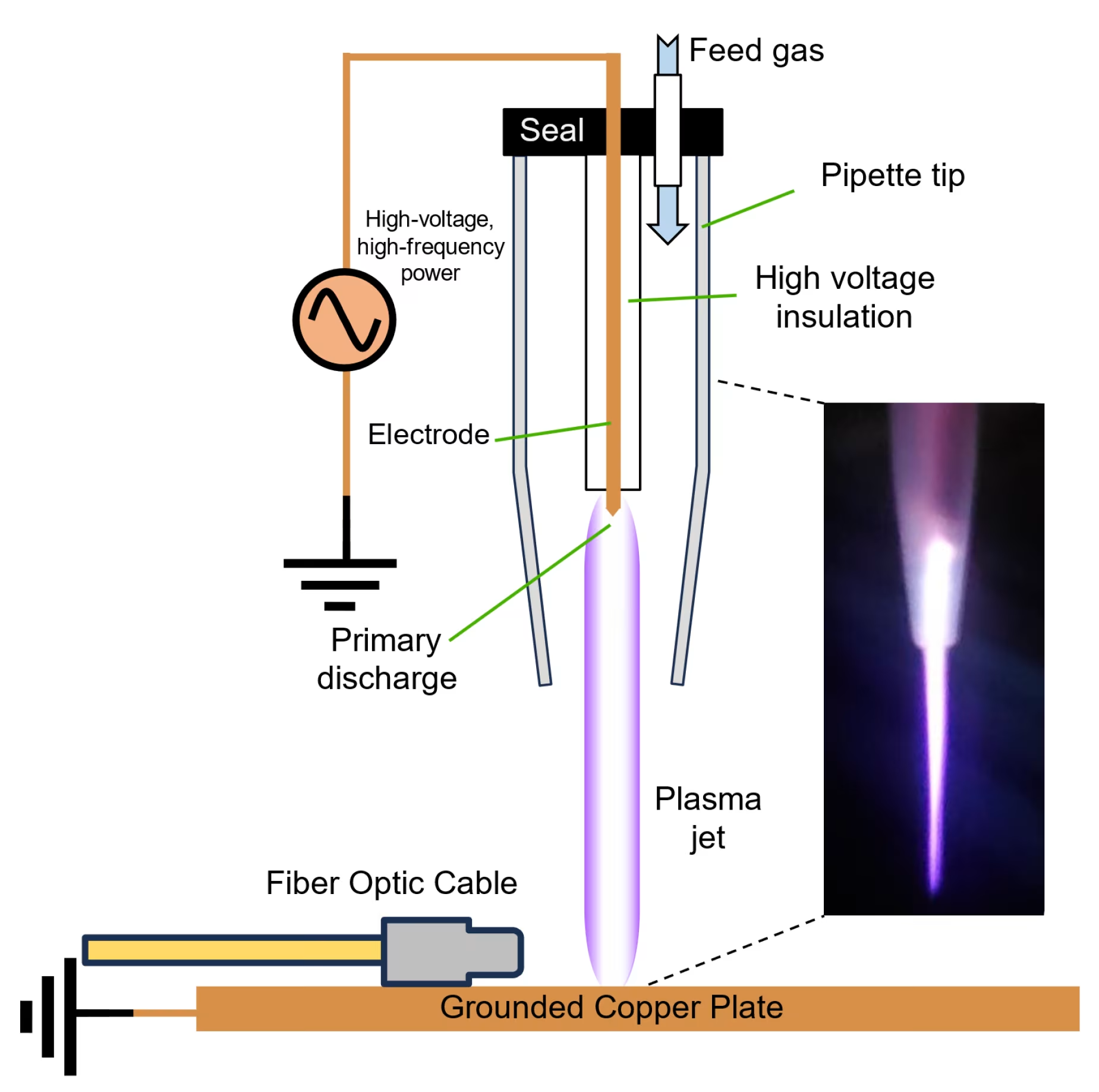
Cold atmospheric plasma operates through multiple interconnected biological pathways that directly address the complex challenges of pressure ulcer healing. The technology creates a controlled environment of reactive species, including reactive oxygen species (ROS) and reactive nitrogen species (RNS), which interact with wound tissues to promote healing[1].
When applied to pressure ulcers, cold plasma generates physiologically relevant concentrations of these bioactive molecules that stimulate cellular repair mechanisms. Research demonstrates that CAP treatment significantly increases the activity of antioxidant enzymes including catalase, superoxide dismutase, and glutathione peroxidase in wound tissues[2].
Nitric Oxide Production in Pressure Ulcer Healing
One of the most significant mechanisms involves the controlled production of nitric oxide (NO), which plays crucial roles in wound healing and tissue repair. Cold plasma treatment increases endothelial nitric oxide synthase (eNOS) expression, leading to enhanced NO production that affects vascular function and tissue regeneration processes[3].
The Mirari Cold Plasma System, developed by General Vibronics and commercialized by Mirari Doctor, utilizes proprietary nitric oxide-based technology that distinguishes it from traditional ROS-based systems. This approach provides enhanced safety profiles while maintaining therapeutic efficacy for pressure ulcer applications, particularly in promoting circulation and reducing inflammation.
Addressing Pressure Ulcer Pathophysiology
Cold plasma therapy targets multiple pathophysiological processes that contribute to pressure ulcer development and persistence. The technology has been shown to reduce inflammatory cytokine levels, improve tissue oxygenation, and enhance cellular proliferation in wound areas[4].
Studies indicate that cold plasma treatment can significantly reduce oxidative stress markers and promote the expression of growth factors essential for tissue repair. This comprehensive approach addresses both the immediate wound healing needs and the underlying factors that contribute to pressure ulcer chronicity.
Clinical Evidence for Cold Plasma in Pressure Ulcer Treatment
Randomized Clinical Trial Outcomes
Clinical research has demonstrated significant benefits of cold plasma for pressure ulcers across multiple studies. A landmark study involving 50 patients with pressure ulcers showed that weekly cold plasma treatments for eight weeks resulted in significantly better healing outcomes compared to standard care alone[5].
The study found that improvement, including bacterial load decrease, was significantly greater in the CAP group after just the first week of treatment. Patients receiving cold plasma therapy showed accelerated wound healing, reduced wound size, and improved tissue quality compared to conventional treatment approaches.
Real-World Case Study Results
A compelling case study involved a 66-year-old patient with a complex pressure ulcer who experienced remarkable healing with cold plasma therapy. After multiple failed conventional treatments, cold plasma application resulted in a 43% reduction in wound area within 30 days, demonstrating the technology’s potential for treatment-resistant cases[6].
The case study also documented significant bacterial load reduction from grade 3 to grade 1, highlighting the antimicrobial effectiveness of cold plasma therapy. This dual action of promoting healing while controlling infection represents a major advantage for pressure ulcer management.
Systematic Review and Meta-Analysis Findings
Recent systematic reviews have evaluated the effectiveness of cold plasma for pressure ulcers and other chronic wounds. A comprehensive analysis found that cold plasma therapy consistently accelerated wound healing, reduced wound size, and promoted tissue regeneration across multiple studies[7].
The review noted that all studies reported no adverse side effects or safety concerns with cold plasma treatment, establishing an excellent safety profile for this innovative therapy. This safety advantage is particularly important for pressure ulcer patients who often have compromised health status and multiple comorbidities.
Technical Specifications of Cold Plasma Pressure Ulcer Treatment
| Parameter | Specification | Clinical Application |
|---|---|---|
| Operating Temperature | Room temperature (20-25°C) | Safe for compromised skin and tissue |
| Treatment Duration | 1-2 minutes per cm² | Customizable based on ulcer size |
| Session Frequency | 1-3 times weekly | Optimized for pressure ulcer healing |
| Reactive Species | NO, ROS, RNS production | Multiple therapeutic mechanisms |
| Antimicrobial Activity | Broad-spectrum pathogen reduction | Effective against resistant bacteria |
| Penetration Depth | 2-5mm tissue penetration | Reaches deeper ulcer tissues |
Clinical Benefits and Treatment Outcomes
| Pressure Ulcer Stage | Treatment Protocol | Reported Outcomes | Timeline |
|---|---|---|---|
| Stage II Ulcers | Weekly for 8 weeks | Significant size reduction, improved healing | 2-4 weeks |
| Stage III Ulcers | 2-3 times weekly | Enhanced granulation tissue formation | 4-8 weeks |
| Infected Ulcers | Daily until infection clears | Rapid bacterial load reduction | 1-2 weeks |
| Chronic Non-healing | 3 times weekly for 4 weeks | Accelerated healing progression | 3-6 weeks |
| Post-surgical Sites | 2 times weekly | Reduced complications, faster closure | 2-4 weeks |
| Complex Wounds | Individualized protocols | Improved tissue quality and healing | Variable |
Antimicrobial Effects in Pressure Ulcers
One of the most significant advantages of cold plasma for pressure ulcers is its powerful antimicrobial activity. Research shows that CAP treatment effectively reduces bacterial load, particularly problematic organisms like Staphylococcus aureus and Pseudomonas aeruginosa commonly found in pressure ulcer infections[8].
Clinical studies have demonstrated immediate antiseptic effects following cold plasma treatment, helping prevent the progression to serious infections that could complicate healing. This antimicrobial effect occurs through multiple mechanisms including membrane disruption and protein denaturation in pathogenic microorganisms.
Tissue Regeneration and Healing Enhancement
Cold plasma therapy promotes tissue regeneration through multiple pathways including enhanced angiogenesis, increased collagen synthesis, and improved cellular proliferation. Studies show that cold plasma treatment significantly accelerates re-epithelialization and promotes the formation of healthy granulation tissue[9].
The technology’s ability to stimulate growth factor production and enhance cellular migration creates an optimal environment for pressure ulcer healing. Patients often experience improved wound bed preparation and faster progression through the healing phases.
Safety Profile and Patient Experience
Excellent Safety Record in Vulnerable Populations
Cold plasma therapy demonstrates an outstanding safety profile in pressure ulcer patients, who often represent vulnerable populations with multiple comorbidities. Clinical trials consistently report minimal adverse effects, with most patients experiencing no discomfort during treatment[10].
The non-thermal nature of cold plasma therapy makes it particularly suitable for patients with compromised circulation or sensation, common issues in pressure ulcer populations. Unlike thermal treatments that could cause additional tissue damage, cold plasma operates at room temperature, eliminating burn risks.
Patient Tolerance and Comfort
Patients typically describe cold plasma treatment as comfortable, with many reporting a mild tingling sensation or slight warmth during application. The therapy can be administered in various healthcare settings without the need for anesthesia or special preparation, making it accessible for patients with mobility limitations.
Healthcare providers report high patient acceptance rates and compliance with cold plasma treatment protocols. The non-invasive nature and minimal side effects make it an attractive option for patients who may be reluctant to undergo more aggressive interventions.
Comparing Cold Plasma to Traditional Pressure Ulcer Treatments
Advantages Over Conventional Wound Care
Cold plasma for pressure ulcers offers several distinct advantages over traditional treatment approaches. Unlike debridement procedures that can be painful and may remove healthy tissue along with damaged areas, cold plasma selectively targets pathological processes while preserving healthy tissue[11].
The technology’s antimicrobial effects are particularly valuable in pressure ulcer care, where infection control is crucial. Traditional antibiotic treatments may be less effective due to biofilm formation and the presence of resistant organisms. Cold plasma can penetrate biofilms and eliminate bacteria without promoting antibiotic resistance.
Cost-Effectiveness and Healthcare Outcomes
From a healthcare economics perspective, cold plasma therapy may offer significant cost savings by reducing the need for more expensive interventions. By accelerating wound healing and preventing complications, CAP treatment can help patients avoid prolonged hospitalizations and complex surgical procedures.
The Mirari Cold Plasma System’s portability and ease of use make it particularly valuable for pressure ulcer care, as it can be used in various healthcare settings including long-term care facilities and home healthcare environments. This accessibility could help expand treatment options for pressure ulcer patients in diverse care settings.
Implementation and Clinical Protocols
Patient Selection Criteria
Ideal candidates for cold plasma pressure ulcer treatment include patients with Stage II-IV pressure ulcers who have not responded adequately to conventional therapies. The technology is particularly beneficial for patients with infected ulcers, chronic non-healing wounds, or those at high risk for complications.
Healthcare providers should assess patient suitability based on ulcer characteristics, overall health status, and treatment goals. The non-invasive nature of cold plasma makes it suitable for most patients, including those who may not be candidates for surgical interventions.
Treatment Protocol Development
Effective cold plasma treatment requires careful protocol development based on individual patient needs and ulcer characteristics. Healthcare providers typically begin with 1-3 treatments per week, adjusting frequency based on patient response and healing progression.
Treatment duration varies based on ulcer size and severity, with typical sessions lasting 1-2 minutes per square centimeter of wound area. The Mirari Cold Plasma System’s adjustable parameters allow practitioners to customize treatments based on patient tolerance and specific healing requirements.
Future Directions and Research Developments
Emerging Applications and Protocols
Research into cold plasma applications for pressure ulcers continues to expand, with new protocols being developed for specific patient populations and wound types. Current investigations include optimized treatment parameters for different pressure ulcer stages and combination therapies with other wound care modalities.
Scientists are working to develop more sophisticated treatment algorithms that can predict optimal cold plasma parameters based on wound characteristics and patient factors. This personalized approach could further enhance treatment outcomes and efficiency.
Integration with Advanced Wound Care
Future developments may include integration of cold plasma therapy with other advanced wound care technologies, such as negative pressure wound therapy, bioengineered tissues, and smart wound dressings. These combination approaches could provide synergistic benefits for complex pressure ulcer cases.
The growing body of research supporting cold plasma therapy for pressure ulcers has attracted attention from healthcare providers and wound care specialists seeking alternatives to conventional treatments. As more clinical data becomes available, the technology is likely to play an increasingly important role in comprehensive pressure ulcer management.
Patient-Focused Frequently Asked Questions
Is cold plasma therapy safe for all pressure ulcer patients?
Cold plasma therapy has an excellent safety profile for most pressure ulcer patients, including those with compromised circulation, diabetes, or multiple comorbidities. Clinical studies consistently show minimal adverse effects, with most patients experiencing no discomfort during treatment. However, patients with active infections requiring immediate surgical intervention, certain medical implants near the treatment site, or severe cardiovascular instability should be evaluated carefully before treatment. Healthcare providers will assess individual suitability and monitor patients throughout the treatment course to ensure safety and effectiveness.
How quickly can patients see results from cold plasma treatment?
Most pressure ulcer patients begin to notice improvements in wound appearance and healing within the first week of cold plasma treatment. Significant wound size reduction typically becomes apparent within 2-4 weeks of consistent treatment, though this varies based on ulcer severity, patient health status, and wound characteristics. The antimicrobial effects are often immediate, with bacterial load reduction observable within 24-48 hours. Patients with smaller, less severe ulcers generally experience faster healing responses, while complex or chronic wounds may require longer treatment courses.
Can cold plasma therapy replace traditional pressure ulcer treatments?
Cold plasma therapy is designed to complement, not replace, comprehensive pressure ulcer management strategies. While research shows that CAP treatment can significantly accelerate healing and reduce complications, it should be used as part of a comprehensive care plan that includes pressure relief, proper nutrition, wound cleaning, and appropriate dressings. The technology enhances traditional treatments by providing antimicrobial effects and stimulating healing processes that conventional methods cannot achieve alone.
How does cold plasma treatment compare to other advanced wound therapies?
Cold plasma therapy offers several advantages over other advanced wound treatments for pressure ulcers. Unlike negative pressure wound therapy, which requires complex equipment and may cause discomfort, cold plasma provides gentle, non-invasive treatment with minimal setup requirements. Compared to growth factor therapies or bioengineered tissues, CAP offers immediate antimicrobial effects while stimulating natural healing processes. The therapy also provides broader benefits than single-mechanism treatments, addressing infection control, inflammation reduction, and tissue regeneration simultaneously.
What should patients expect during cold plasma treatment sessions?
During cold plasma treatment, pressure ulcer patients typically experience a mild tingling sensation or slight warmth at the treatment site. Sessions usually last 5-15 minutes depending on ulcer size and are performed in comfortable healthcare settings without special preparation. Most patients find the treatment relaxing and well-tolerated. After treatment, patients can immediately resume normal activities, though they should follow any specific wound care instructions provided by their healthcare team. Some patients may notice slight changes in wound appearance immediately after treatment, which typically indicates positive healing responses.
Medical Disclaimer: This information is for educational purposes only and should not replace professional medical advice. Pressure ulcer patients should always consult with qualified healthcare providers before starting any new treatment. Individual responses to cold plasma therapy may vary, and treatment decisions should be based on comprehensive medical evaluation and ongoing wound care management needs.
References
- Raissi-Dehkordi, N., et al. (2025). Advancing chronic and acute wound healing with cold atmospheric plasma. Frontiers in Medicine. https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1527736/full
- Bolgeo, T., et al. (2023). The Role of Cold Atmospheric Plasma in Wound Healing Processes in Critically Ill Patients. PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC10219374/
- Arndt, S., et al. (2019). Cold atmospheric plasma modulates endothelial nitric oxide synthase signalling and enhances burn wound neovascularisation. Journal of Pathology. https://pubmed.ncbi.nlm.nih.gov/31265742/
- Braný, D., et al. (2020). Cold Atmospheric Plasma: A Powerful Tool for Modern Medicine. PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC7215620/
- Braný, D., et al. (2020). Cold Atmospheric Plasma: A Powerful Tool for Modern Medicine. PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC7215620/
- Athenaeum Publishing. (2024). Use of Cold Plasma in the Treatment of Infected Wounds. https://athenaeumpub.com/use-of-cold-plasma-in-the-treatment-of-infected-wounds/
- PMC. (2025). Cold Atmospheric Pressure Plasma in the Treatment of Diabetic Foot Ulcers. https://pmc.ncbi.nlm.nih.gov/articles/PMC12050158/
- Nature. (2020). Cold atmospheric plasma as an effective method to treat diabetic foot ulcers. https://www.nature.com/articles/s41598-020-67232-x
- Nature. (2018). In vivo study of non-invasive effects of non-thermal plasma on pressure ulcer treatment. https://www.nature.com/articles/s41598-018-24049-z
- JAMA Network Open. (2020). Effect of Cold Atmospheric Plasma Therapy vs Standard Therapy Placebo on Wound Healing in Patients With Diabetic Foot Ulcers. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2768340
- Mirari Doctor. (2025). Wound Healing: Revolutionary Cold Plasma Technology. https://miraridoctor.com/wound-healing/
Related articles
Made in USA