Imagine a pain so intense that even the lightest touch feels like a searing flame. For millions of people worldwide, this is the reality of living with neuropathic pain, a debilitating condition that arises from damage to the nervous system[1]. But what if there was a cutting-edge treatment that could provide lasting relief without the side effects of traditional medications? Enter Mirari Cold Plasma, a groundbreaking technology developed by General Vibronics that harnesses the power of nitric oxide (NO). In this comprehensive guide, we’ll explore the complex world of neuropathic pain and discover how Mirari Cold Plasma is revolutionizing patient care.
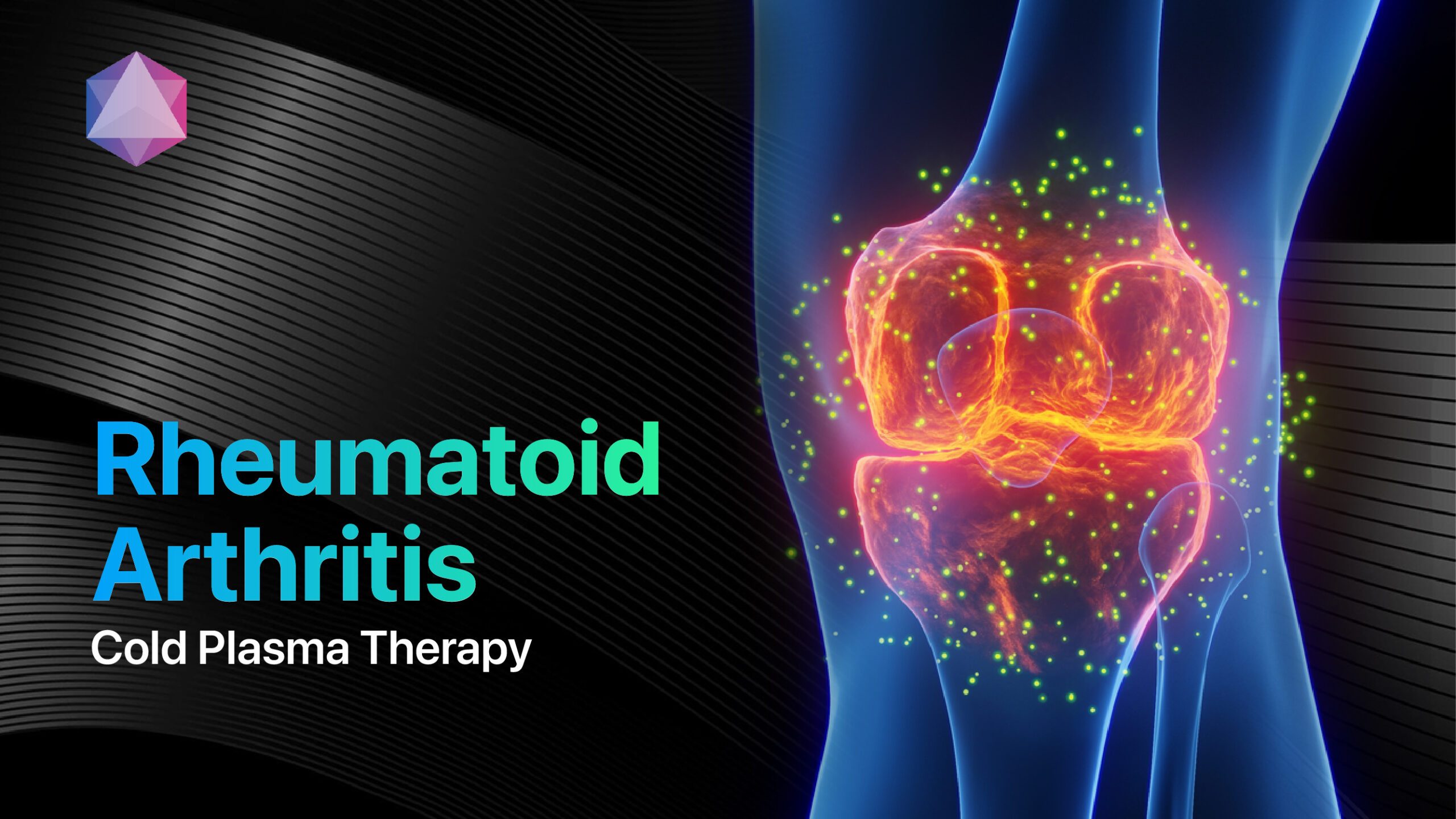
1. What is Neuropathic Pain?
Definition of Neuropathic Pain
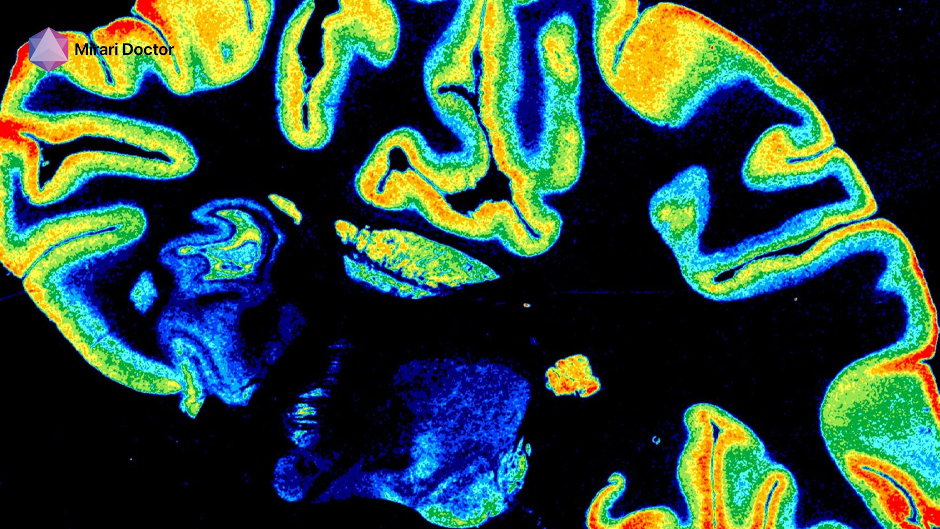
Neuropathic pain is a type of chronic pain that occurs due to damage or dysfunction of the nervous system, including the nerves, spinal cord, and brain. Unlike nociceptive pain, which is caused by actual tissue damage, neuropathic pain arises from abnormal signaling within the nervous system itself[1].
Neuropathic pain is chronic pain from nervous system damage or dysfunction.
Mechanisms Behind Neuropathic Pain
The exact mechanisms underlying neuropathic pain are complex and not fully understood, but they involve a combination of peripheral and central nervous system processes. Some key factors include:
- Sensitization of nociceptors (pain receptors) in the peripheral nerves[2]
- Abnormal firing of damaged or dysfunctional nerves[2]
- Changes in neurotransmitter levels and receptor expression[2]
- Alterations in the processing and modulation of pain signals in the spinal cord and brain[2]
- Activation of glial cells (non-neuronal cells in the nervous system) that contribute to inflammation and pain[2]
These mechanisms can lead to a state of central sensitization, where the nervous system becomes hyperexcitable and amplifies pain signals, even in the absence of ongoing tissue damage[2].
Types of Neuropathic Pain Conditions
Neuropathic pain can arise from a wide range of conditions that affect the nervous system, including:
- Diabetic neuropathy[3]
- Postherpetic neuralgia (pain after shingles)[3]
- Trigeminal neuralgia[3]
- Chemotherapy-induced peripheral neuropathy[3]
- HIV-associated neuropathy[3]
- Phantom limb pain[3]
- Multiple sclerosis[3]
- Spinal cord injury[3]
- Stroke[3]
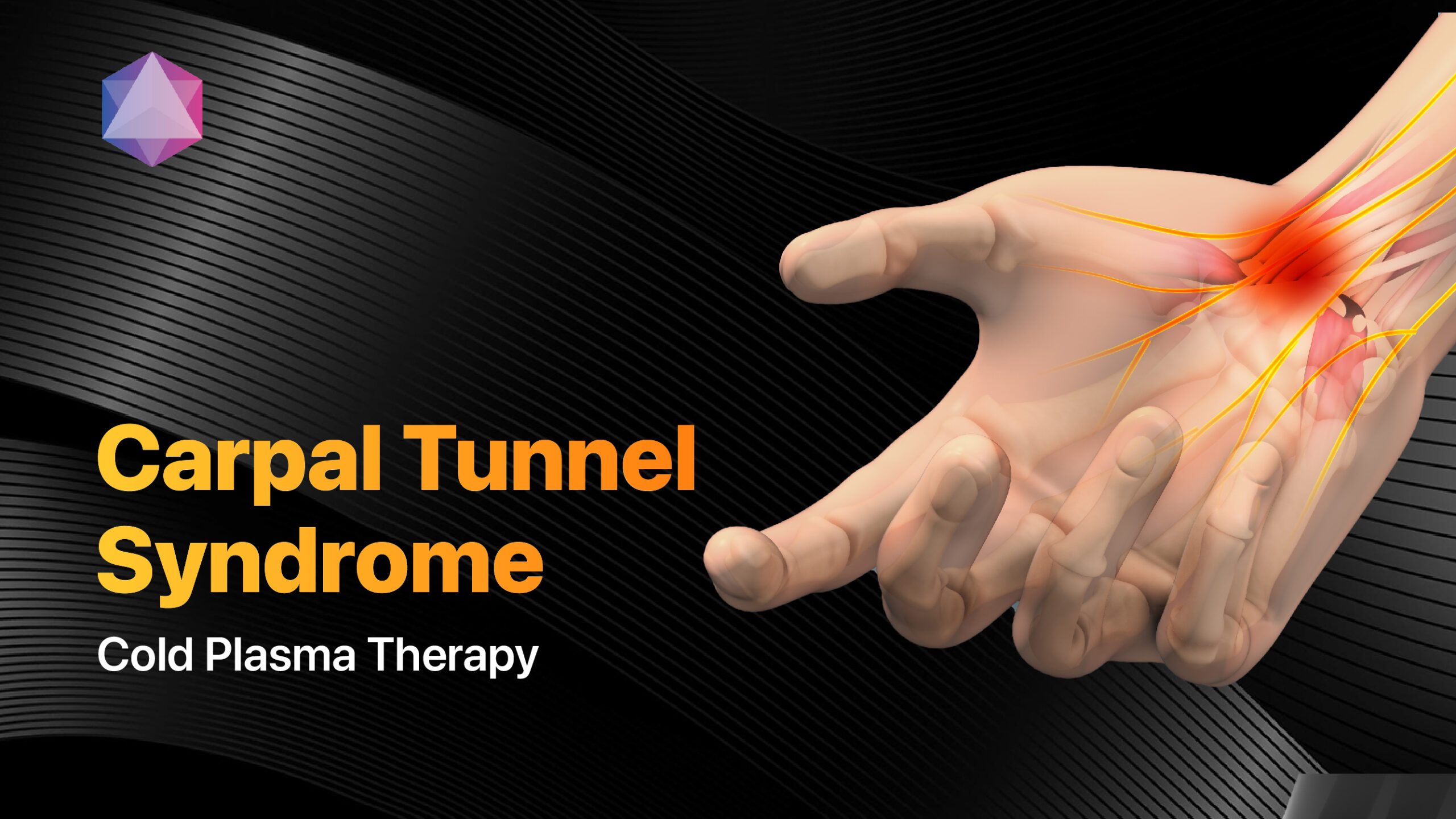
- Carpal tunnel syndrome[3]
Each of these conditions can cause distinct patterns of neuropathic pain, depending on the location and extent of nervous system damage[3].

Postherpetic neuralgia
Symptoms of Neuropathic Pain
The symptoms of neuropathic pain can vary widely between individuals but often include:
- Burning, shooting, or electric shock-like sensations[1]
- Tingling or “pins and needles” feelings[1]
- Numbness or reduced sensation in the affected area[1]
- Allodynia (pain from normally non-painful stimuli, such as light touch)[1]
- Hyperalgesia (increased sensitivity to painful stimuli)[1]
- Spontaneous pain (pain that occurs without any apparent trigger)[1]
These symptoms can be constant or intermittent and may fluctuate in intensity over time. They can significantly impact quality of life, leading to sleep disturbances, anxiety, depression, and disability[1].

Neuropathic pain symptoms include burning, tingling, and heightened sensitivity, significantly affecting quality of life.
Differentiating Neuropathic Pain from Other Pain Types
Distinguishing neuropathic pain from other types of pain is crucial for accurate diagnosis and treatment. Some key features that suggest a neuropathic component include:
- Pain that is described as burning, shooting, or electric shock-like[1]
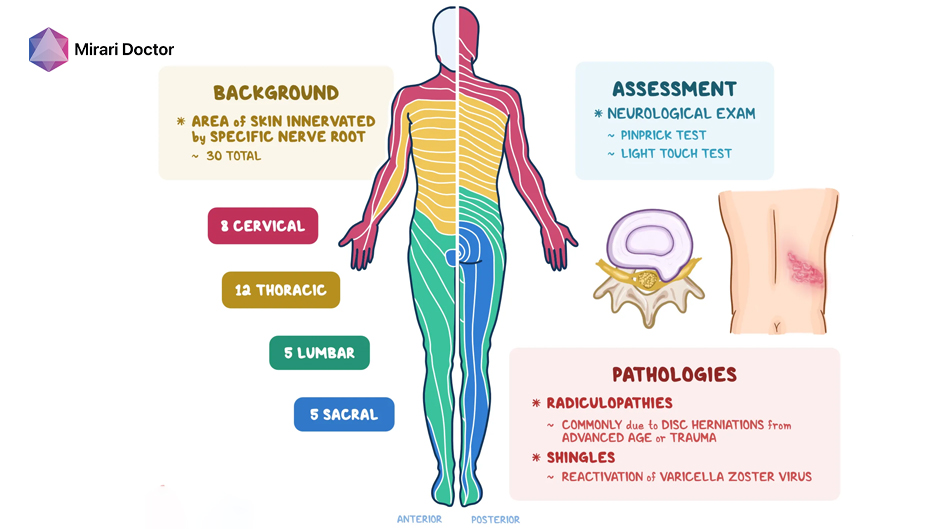
- Pain that follows the distribution of a specific nerve or dermatome (skin area innervated by a specific spinal nerve)[1]
- Presence of sensory abnormalities, such as allodynia or hyperalgesia[1]
- Lack of response to traditional analgesics, such as acetaminophen or ibuprofen[1]
However, neuropathic pain can coexist with other types of pain, such as nociceptive or inflammatory pain, making the clinical picture more complex. A thorough assessment by a pain specialist is often necessary to accurately diagnose and classify the pain[1].
2. Causes of Neuropathic Pain
 |
Common Medical Conditions Leading to Neuropathic PainMany medical conditions can lead to neuropathic pain by causing damage or dysfunction of the nervous system. Some of the most common include:
Other conditions, such as vitamin deficiencies, alcoholism, or autoimmune disorders, can also contribute to the development of neuropathic pain[1]. |
 |
Role of Nerve Injury and DamageNerve injury or damage is a key factor in the development of neuropathic pain. This can occur through various mechanisms, including:
When nerves are injured or damaged, they can undergo a process called Wallerian degeneration, where the distal portion of the nerve (the part furthest from the cell body) degenerates and is cleared by immune cells[4]. This process can trigger a cascade of cellular and molecular changes that contribute to the development of neuropathic pain, such as the upregulation of pain-related genes and the infiltration of inflammatory cells[4]. |
 |
Medications That Can Induce Neuropathic PainCertain medications can cause or exacerbate neuropathic pain as a side effect. Some examples include:
The mechanisms by which these medications cause neuropathic pain are not fully understood but may involve direct neurotoxicity, mitochondrial dysfunction, or altered ion channel function[4]. |
 |
Lifestyle Factors Contributing to Neuropathic PainCertain lifestyle factors can increase the risk of developing neuropathic pain or exacerbate existing pain. These include:
Modifying these lifestyle factors, along with managing underlying medical conditions, can help prevent or mitigate the development of neuropathic pain[1]. |
3. Diagnosis of Neuropathic Pain
Clinical History and Symptom Assessment
Diagnosing neuropathic pain begins with a thorough clinical history and assessment of symptoms. Key elements include:
- Characterization of pain: Patients are asked to describe the quality, intensity, location, and temporal pattern of their pain, as well as any aggravating or alleviating factors[1].
- Identification of sensory abnormalities: Patients are asked about the presence of allodynia, hyperalgesia, or other sensory disturbances in the affected area[1].
- Review of medical history: The clinician inquires about any pre-existing medical conditions, medications, or surgical procedures that may contribute to neuropathic pain[1].
- Assessment of functional impact: Patients are asked about the effects of pain on their daily activities, sleep, mood, and overall quality of life[1].
This information helps the clinician determine the likelihood of a neuropathic pain component and guides further diagnostic testing.

Diagnosing neuropathic pain involves evaluating pain characteristics, sensory issues, and medical history.
Diagnostic Tools and Tests
Several diagnostic tools and tests can be used to confirm the presence of neuropathic pain and identify the underlying cause. These include:
- Neurological examination: A comprehensive neurological exam assesses sensory function, reflexes, and motor strength to detect signs of nerve damage or dysfunction[2].
- Quantitative sensory testing (QST): QST uses standardized stimuli to measure sensory thresholds and detect abnormalities in pain processing[7].
- Nerve conduction studies (NCS) and electromyography (EMG): These tests assess the function of peripheral nerves and muscles to identify the location and extent of nerve damage[7].
- Skin biopsy: A small skin sample is analyzed for the presence and density of small nerve fibers, which can be reduced in neuropathic pain conditions[7].
- Imaging studies: MRI, CT, or ultrasound can be used to visualize structural abnormalities or compression of nerves, spinal cord, or brain[2].
- Blood tests: Laboratory tests can help identify underlying conditions that may contribute to neuropathic pain, such as diabetes, vitamin deficiencies, or autoimmune disorders[2].
The specific tests ordered will depend on the individual’s clinical presentation and the suspected underlying cause of neuropathic pain.

A neurological exam evaluates sensory function, reflexes, and motor strength to detect nerve damage.
Importance of Neuroanatomical Patterns in Diagnosis
Recognizing the neuroanatomical patterns of pain and sensory abnormalities is crucial for accurately diagnosing neuropathic pain. Some key patterns include:
- Dermatomal distribution: Pain or sensory changes that follow the distribution of a specific spinal nerve root, as in radiculopathy or postherpetic neuralgia[8].
- Peripheral nerve distribution: Pain or sensory changes that follow the distribution of a specific peripheral nerve, as in carpal tunnel syndrome or diabetic neuropathy[8].
- Glove-and-stocking distribution: Symmetrical sensory changes in the distal extremities, as in length-dependent polyneuropathies[8].
- Hemibody distribution: Pain or sensory changes affecting one side of the body, as in central post-stroke pain or multiple sclerosis[8].
These patterns can help localize the site of nervous system damage and guide further diagnostic testing and treatment decisions[8].
Challenges in Diagnosing Neuropathic Pain
Diagnosing neuropathic pain can be challenging for several reasons:
- Overlap with other pain types: Neuropathic pain often coexists with nociceptive or inflammatory pain, making it difficult to distinguish the specific components[9].
- Variability in presentation: The symptoms and neuroanatomical patterns of neuropathic pain can vary widely between individuals, even with the same underlying condition[9].
- Lack of objective biomarkers: There are currently no widely accepted objective biomarkers for neuropathic pain, making diagnosis reliant on clinical assessment and patient-reported outcomes[9].
- Comorbidities: Many patients with neuropathic pain have multiple comorbid conditions, such as depression, anxiety, or sleep disorders, which can complicate the diagnostic process[9].
Overcoming these challenges requires a multidisciplinary approach that combines careful clinical assessment, appropriate diagnostic testing, and consideration of the patient’s overall medical and psychosocial context[9].
Diagnosing neuropathic pain is challenging due to symptom overlap and variability.
When to Seek Specialist Evaluation
Patients with suspected neuropathic pain should be referred to a pain specialist or neurologist if:
- The pain is severe, persistent, or significantly impacts quality of life[9].
- The underlying cause of the pain is unclear or complex[9].
- The pain does not respond to initial treatment attempts[9].
- There are concerns about medication side effects or interactions[9].
- The patient has significant comorbidities or psychosocial factors that complicate management[9].
Early referral to a specialist can help ensure accurate diagnosis, optimize treatment, and prevent the development of chronic pain and disability[9].

Refer to a specialist if neuropathic pain is severe, persistent, unclear, unresponsive to treatment, or complicated by comorbidities.
4. Treatment Options for Neuropathic Pain
Pharmacological Treatments
Pharmacological treatments are the mainstay of neuropathic pain management and include several classes of medications with distinct mechanisms of action.
Antidepressants
Tricyclic antidepressants (TCAs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) are commonly used to treat neuropathic pain. These medications work by increasing the levels of neurotransmitters, such as serotonin and norepinephrine, which can modulate pain signaling in the spinal cord and brain. Examples include:
- TCAs: Amitriptyline, nortriptyline, desipramine
- SNRIs: Duloxetine, venlafaxine, milnacipran
These medications are typically started at low doses and gradually titrated up to achieve pain relief while minimizing side effects, such as dry mouth, constipation, or sedation[10][11].

TCAs and SNRIs treat neuropathic pain by increasing neurotransmitters that modulate pain signaling.
Anticonvulsants
Anticonvulsants, particularly gabapentinoids, are another first-line treatment for neuropathic pain. These medications work by binding to voltage-gated calcium channels and reducing the release of excitatory neurotransmitters, such as glutamate and substance P. Examples include:
- Gabapentin
- Pregabalin
These medications are also started at low doses and titrated up based on pain relief and tolerability. Common side effects include dizziness, somnolence, and peripheral edema[12][13].
Gabapentinoids treat neuropathic pain by reducing excitatory neurotransmitter release.
Topical Agents
Topical agents can be used to provide localized pain relief with minimal systemic side effects. Examples include:
- Lidocaine patches: These patches contain the local anesthetic lidocaine and can be applied directly to the painful area to provide numbness and pain relief[14].
- Capsaicin cream: This cream contains the active ingredient in chili peppers and works by depleting substance P, a neurotransmitter involved in pain signaling[14].
Topical agents are generally well-tolerated but may cause local skin irritation or burning sensations[14].

Lidocaine patches provide localized numbness and pain relief by applying lidocaine directly to the painful area.
Opioids
Opioids are a class of medications that bind to opioid receptors in the nervous system and can provide powerful pain relief. However, their use in neuropathic pain is controversial due to the risks of addiction, abuse, and overdose. Examples include:
- Morphine
- Oxycodone
- Tramadol
Opioids are generally reserved for cases of severe, refractory neuropathic pain and should be used with caution and close monitoring. They are often combined with other medications, such as antidepressants or anticonvulsants, to achieve optimal pain relief[11][13].

Opioids are used cautiously for severe neuropathic pain due to addiction risks, often with other medications.
Non-Pharmacological Approaches
Non-pharmacological approaches can be used in conjunction with medications to provide comprehensive neuropathic pain management.
 |
Physical TherapyPhysical therapy can help improve function, reduce pain, and prevent further nerve damage in patients with neuropathic pain. Techniques may include:
Physical therapy should be tailored to the individual’s specific condition and goals and may require modification as the pain evolves over time. |
 |
Psychological Support and CounselingNeuropathic pain can have a significant impact on mental health and quality of life, leading to depression, anxiety, and social isolation. Psychological support and counseling can help patients cope with these challenges and develop effective pain management strategies. Approaches may include:
Psychological interventions can be delivered individually or in group settings and may be combined with other therapies, such as medication management or physical therapy. |
 |
Complementary and Alternative MedicineComplementary and alternative medicine (CAM) approaches can be used to supplement conventional treatments for neuropathic pain. Examples include:
While some CAM approaches have shown promise in managing neuropathic pain, the evidence for their effectiveness is often limited, and they should be used with caution and under the guidance of a healthcare provider. |
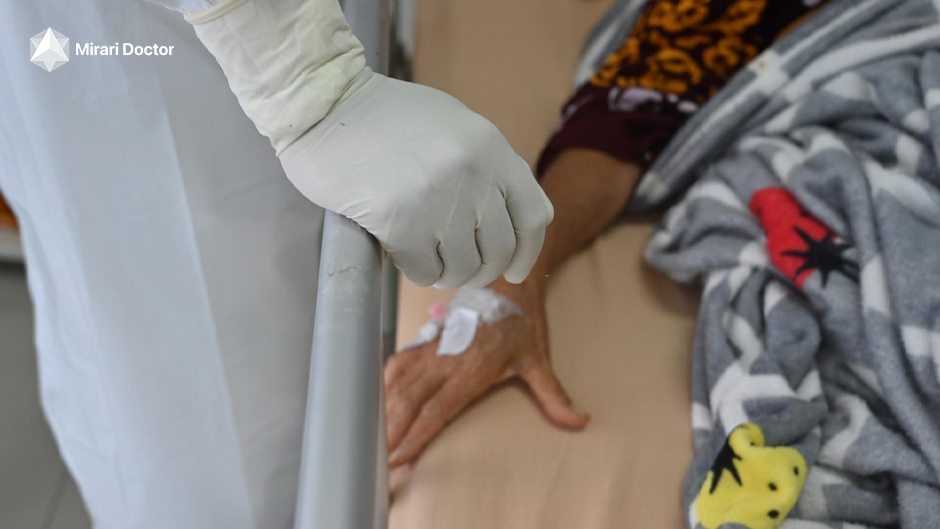
Cold Plasma Therapy
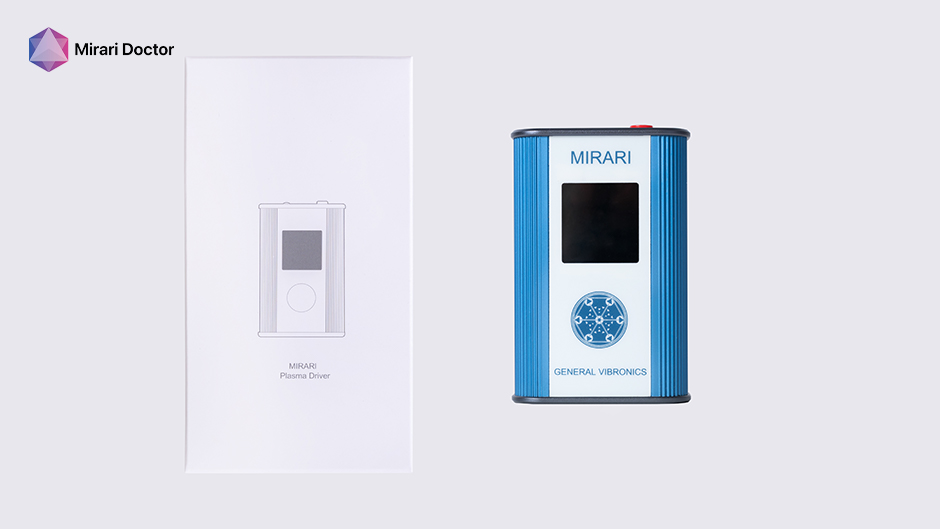
Cold plasma therapy, particularly Mirari Cold Plasma developed by General Vibronics, is an innovative treatment approach that harnesses the power of nitric oxide (NO) to provide targeted relief for neuropathic pain[18].
Mechanism of Action in Neuropathic Pain Relief: Nitric oxide is a signaling molecule that plays a crucial role in regulating pain processing, inflammation, and nerve function. When applied to the skin via a handheld device, Mirari Cold Plasma generates a precise, controlled dose of NO that can:
- Modulate pain signaling pathways in the peripheral and central nervous system, reducing the transmission of pain signals to the brain[18].
- Reduce inflammation and oxidative stress in the affected nerves, promoting healing and preventing further damage[18].
- Improve blood flow and oxygenation to the nerves, supporting their metabolic needs and facilitating repair[18].
- Stimulate the release of endogenous opioids and other pain-relieving compounds in the body[18].
Potential Benefits and Limitations: Mirari Cold Plasma offers a non-invasive, targeted approach to treating neuropathic pain, without the systemic side effects associated with oral medications. The therapy is generally well-tolerated, with few reported adverse effects, and can be administered in a clinical setting or at home with proper training[18].
However, as with any emerging therapy, more research is needed to fully establish the long-term efficacy and safety of cold plasma therapy in neuropathic pain management. Additionally, while many patients experience significant pain relief with Mirari Cold Plasma, individual responses may vary depending on the specific type and severity of neuropathic pain[18].
Current Research and Future Directions: Cold plasma therapy for neuropathic pain is an active area of research, with ongoing studies investigating its mechanisms of action, optimal treatment protocols, and potential synergies with other therapies. Some key areas of focus include:
- Elucidating the molecular and cellular pathways by which NO modulates pain signaling and promotes nerve repair[18].
- Comparing the effectiveness of cold plasma therapy to established treatments, such as medications or physical therapy, in different types of neuropathic pain[18].
- Evaluating the long-term outcomes and potential for preventing the progression of neuropathic pain with regular cold plasma treatments[18].
- Exploring the use of cold plasma therapy in combination with other non-pharmacological approaches, such as psychological interventions or complementary therapies[18].
As more evidence accumulates, cold plasma therapy, particularly Mirari Cold Plasma, may become an increasingly valuable tool in the multimodal management of neuropathic pain, offering patients a safe, effective, and non-invasive option for relief[18].

Mirari Cold Plasma therapy uses nitric oxide to provide targeted relief for neuropathic pain.
Advanced Treatment Options
In some cases, neuropathic pain may not respond adequately to conventional pharmacological or non-pharmacological treatments. For these patients, more advanced interventional options may be considered.
Nerve Blocks
Nerve blocks involve injecting a local anesthetic, often combined with a corticosteroid, near a specific nerve or group of nerves to provide temporary pain relief. Examples include:
- Peripheral nerve blocks: These target individual nerves, such as the sciatic or femoral nerve, and can be used to diagnose or treat localized neuropathic pain[19].
- Sympathetic nerve blocks: These target the sympathetic nervous system, which can be involved in certain types of neuropathic pain, such as complex regional pain syndrome (CRPS)[19].
- Neuraxial blocks: These involve injections into the epidural or intrathecal space surrounding the spinal cord and can provide more widespread pain relief[19].
Nerve blocks can be used for diagnostic purposes, to identify the source of neuropathic pain, or for therapeutic purposes, to provide short-term or long-term pain relief[19].
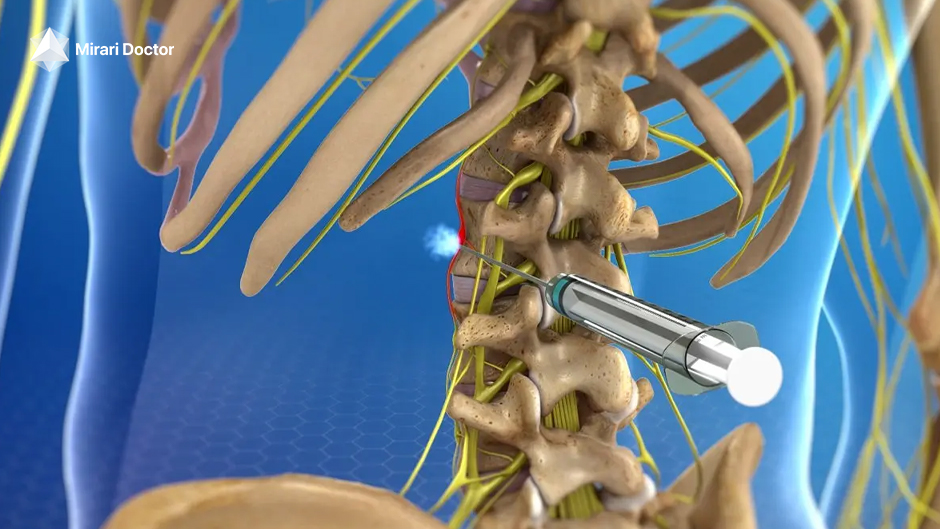
Sympathetic nerve blocks relieve neuropathic pain by targeting the sympathetic nervous system.
Spinal Cord Stimulation
Spinal cord stimulation (SCS) is a neuromodulation technique that involves implanting electrodes in the epidural space near the spinal cord. These electrodes deliver electrical pulses that can modulate pain signaling and provide relief for certain types of neuropathic pain, such as:
- Failed back surgery syndrome[20]
- Complex regional pain syndrome (CRPS)[20]
- Peripheral neuropathy[20]
- Phantom limb pain[20]
SCS is typically reserved for patients who have not responded to more conservative treatments and requires a trial period to assess effectiveness before permanent implantation[20].
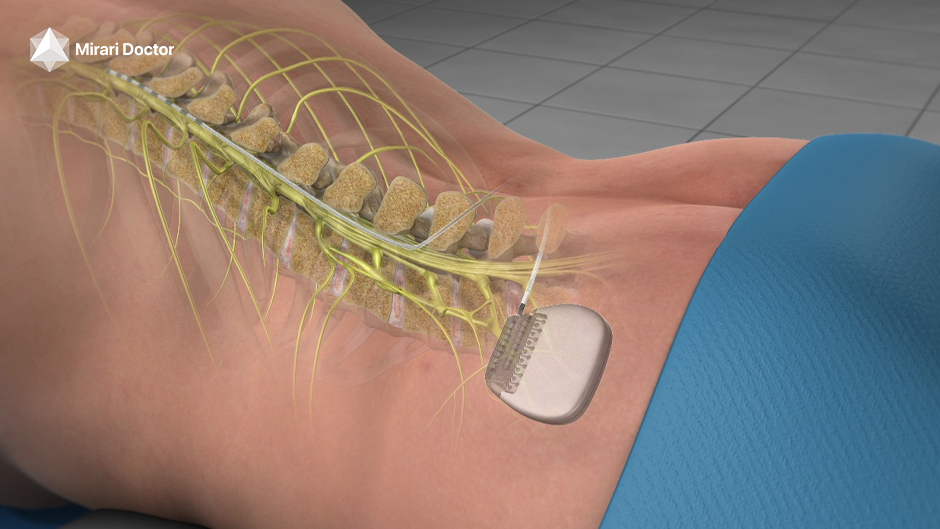
Spinal cord stimulation uses implanted electrodes to modulate pain and relieve neuropathic pain.
Surgical Interventions
In rare cases, surgical interventions may be considered for neuropathic pain that is refractory to other treatments. Examples include:
- Nerve decompression: This involves surgically releasing a compressed or entrapped nerve, as in carpal tunnel syndrome or trigeminal neuralgia[21].
- Nerve resection: This involves cutting or removing a damaged or dysfunctional nerve to prevent the transmission of pain signals[21].
- Dorsal root entry zone (DREZ) lesioning: This involves destroying a specific area of the spinal cord where damaged nerves enter, to disrupt the transmission of pain signals[21].
Surgical interventions for neuropathic pain are generally considered a last resort and require careful patient selection and risk-benefit assessment[21].

Surgical interventions for neuropathic pain are last-resort options and require careful risk assessment.
5. Living with Neuropathic Pain
Strategies for Daily Management
Living with neuropathic pain can be challenging, but there are several strategies that can help patients manage their symptoms and maintain their quality of life.
Pain Management Techniques
In addition to medical treatments, patients can use various techniques to manage their pain on a daily basis. These may include:
- Pacing activities: Breaking up tasks into smaller, manageable parts and taking frequent breaks to avoid overexertion and pain flare-ups[15].
- Relaxation techniques: Practicing deep breathing, progressive muscle relaxation, or visualization exercises to reduce stress and muscle tension[15].
- Heat or cold therapy: Applying heat or cold packs to the affected area to provide temporary pain relief and improve circulation[15].
- Massage or self-massage: Using gentle massage techniques to relax tense muscles and promote relaxation[15].
Patients should work with their healthcare providers to develop a personalized pain management plan that incorporates these techniques alongside medical treatments.

Using gentle massage techniques to relax tense muscles and promote relaxation
Lifestyle Modifications
Making certain lifestyle changes can help patients better manage their neuropathic pain and overall health. These may include:
- Maintaining a healthy diet: Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help support nerve health and reduce inflammation[16].
- Exercising regularly: Engaging in low-impact exercises, such as walking, swimming, or yoga, can improve circulation, reduce stiffness, and boost mood[16].
- Managing stress: Practicing stress-reduction techniques, such as meditation or deep breathing, and engaging in enjoyable activities can help reduce pain and improve coping skills[16].
- Getting enough sleep: Establishing a regular sleep schedule and creating a comfortable sleep environment can help improve sleep quality and reduce pain[16].
- Avoiding triggers: Identifying and avoiding activities or situations that exacerbate pain, such as prolonged standing or exposure to cold temperatures[16].
Patients should work with their healthcare providers to develop a lifestyle plan that is safe and appropriate for their specific condition and needs.

A healthy diet with fruits, vegetables, whole grains, and lean proteins supports nerve health and reduces inflammation.
Incorporating Cold Plasma Therapy in Pain Management Plans
Mirari Cold Plasma therapy can be a valuable addition to a comprehensive neuropathic pain management plan. By delivering precise, controlled doses of nitric oxide (NO) to the affected areas, cold plasma therapy can help:
- Provide targeted pain relief without the systemic side effects of oral medications[18].
- Reduce inflammation and oxidative stress in the nerves, promoting healing and preventing further damage[18].
- Improve blood flow and oxygenation to the nerves, supporting their metabolic needs and facilitating repair[18].
- Enhance the effects of other pain management techniques, such as physical therapy or relaxation exercises[18].
Patients can work with their healthcare providers to determine the optimal frequency and duration of cold plasma therapy sessions based on their individual needs and response to treatment[18].

Mirari Cold Plasma therapy provides targeted pain relief, reduces inflammation, and supports other treatments.
Support Systems and Resources
Living with neuropathic pain can be isolating and emotionally challenging, but patients do not have to face it alone. There are many support systems and resources available to help patients cope with their condition and connect with others who understand their experiences.
- Pain support groups: Joining a local or online support group can provide a sense of community, emotional support, and practical advice from others living with neuropathic pain[1].
- Pain management programs: Many hospitals and clinics offer multidisciplinary pain management programs that provide comprehensive care, including medical treatment, physical therapy, and psychological support[22].
- Patient advocacy organizations: Organizations such as the American Chronic Pain Association or the Neuropathy Association provide education, support, and advocacy for patients with neuropathic pain and other chronic pain conditions[22].
- Online resources: There are many websites, blogs, and forums dedicated to neuropathic pain that offer information, tips, and support from experts and fellow patients[22].
Patients should not hesitate to reach out to their healthcare providers, family, friends, or community resources for support and guidance in managing their neuropathic pain.

Support for neuropathic pain includes support groups, pain management programs, and advocacy organizations.
Coping Mechanisms for Psychological Impact
Neuropathic pain can have a significant psychological impact, leading to depression, anxiety, and reduced quality of life. Developing effective coping mechanisms is crucial for managing these challenges and maintaining emotional well-being.
- Cognitive-behavioral strategies: Learning to identify and challenge negative thoughts, set realistic goals, and engage in positive self-talk can help reduce pain-related distress and improve coping skills[15].
- Mindfulness and acceptance: Practicing mindfulness techniques, such as deep breathing or body scans, and learning to accept pain sensations without judgment can help reduce suffering and improve overall well-being[15].
- Engaging in meaningful activities: Finding ways to engage in enjoyable or meaningful activities, such as hobbies, social interactions, or volunteer work, can help boost mood and provide a sense of purpose[15].
- Seeking professional help: Working with a mental health professional, such as a psychologist or counselor, can provide additional support and guidance in developing coping strategies and addressing the emotional impact of neuropathic pain[15].
Patients should prioritize their emotional well-being and seek help if they are struggling with the psychological effects of neuropathic pain.

Mindfulness and acceptance techniques can reduce suffering and improve well-being by managing pain sensations.
Importance of Nutrition and Exercise
Proper nutrition and regular exercise are essential components of neuropathic pain management and overall health.
- Nutrition: Eating a balanced diet rich in vitamins, minerals, and antioxidants can help support nerve health, reduce inflammation, and promote healing. Some specific nutrients that may be beneficial for neuropathic pain include:
- B vitamins (B1, B6, B12): These vitamins are essential for proper nerve function and may help reduce pain and improve nerve conduction[17].
- Omega-3 fatty acids: These healthy fats, found in fish, nuts, and seeds, have anti-inflammatory properties and may help reduce nerve pain[17].
- Magnesium: This mineral is involved in nerve transmission and may help reduce pain and improve nerve function[17].
- Exercise: Regular physical activity can help improve circulation, reduce stiffness, and boost mood in patients with neuropathic pain. Low-impact exercises, such as walking, swimming, or tai chi, are generally safe and well-tolerated. Benefits of exercise for neuropathic pain include:
- Improved blood flow: Exercise helps increase blood flow to the nerves, delivering oxygen and nutrients and promoting healing[17].
- Reduced inflammation: Regular exercise can help reduce systemic inflammation, which may contribute to neuropathic pain[17].
- Increased endorphins: Exercise stimulates the release of endorphins, the body’s natural pain-relieving and mood-boosting chemicals[17].
- Improved flexibility and strength: Gentle stretching and strengthening exercises can help reduce stiffness, improve range of motion, and support affected nerves[17].
Patients should work with their healthcare providers to develop a safe and appropriate nutrition and exercise plan based on their specific needs and limitations.

Regular low-impact exercise improves blood flow, reduces inflammation, and boosts mood for neuropathic pain relief.
Monitoring and Adjusting Treatment Plans
Neuropathic pain is a complex and dynamic condition that may require ongoing monitoring and adjustment of treatment plans to ensure optimal management.
- Regular follow-up: Patients should schedule regular follow-up appointments with their healthcare providers to assess their pain levels, functional status, and response to treatment[18].
- Tracking symptoms: Keeping a pain diary or using pain assessment tools can help patients and providers track changes in pain intensity, location, and quality over time[18].
- Adjusting medications: Based on the patient’s response and side effects, providers may need to adjust medication dosages, switch to different medications, or add adjunctive therapies to optimize pain relief[18].
- Modifying non-pharmacological approaches: Patients may need to modify their physical therapy, exercise, or other non-pharmacological approaches based on their progress and changing needs[18].
- Incorporating new therapies: As new treatments become available, such as cold plasma therapy, providers may incorporate them into the patient’s management plan to enhance pain relief and overall outcomes[18].
Open communication between patients and their healthcare team is essential for ensuring that treatment plans remain effective and responsive to the patient’s evolving needs and goals[18].

Managing neuropathic pain requires regular follow-ups, tracking symptoms, adjusting treatments, and integrating new therapies.
6. Prevention of Neuropathic Pain
While not all cases of neuropathic pain can be prevented, there are several strategies that can help reduce the risk of developing this condition or minimize its severity.
 |
Lifestyle Modifications to Reduce RiskAdopting a healthy lifestyle can help reduce the risk of developing conditions that contribute to neuropathic pain, such as diabetes, cardiovascular disease, or certain infections.
|
 |
Importance of Regular Health ScreeningRegular health screenings can help detect and manage conditions that may contribute to neuropathic pain, such as diabetes, vitamin deficiencies, or autoimmune disorders.
Early detection and management of these conditions can help prevent or minimize the development of neuropathic pain. |
 |
Managing Underlying Conditions EffectivelyFor patients with conditions that can lead to neuropathic pain, such as diabetes, HIV, or multiple sclerosis, effective management of these underlying conditions is crucial for preventing or minimizing nerve damage.
Working closely with healthcare providers to optimize the management of underlying conditions is essential for reducing the risk and severity of neuropathic pain. |
 |
Educating Patients About Neuropathy RisksPatient education is a key component of neuropathic pain prevention. Healthcare providers should educate patients about the risk factors, signs, and symptoms of neuropathic pain, as well as strategies for reducing their risk.
Empowering patients with knowledge and tools to take an active role in their health can help prevent neuropathic pain and improve overall outcomes. |
 |
Community Support and Awareness ProgramsRaising awareness about neuropathic pain and its risk factors at the community level can help promote prevention and early intervention.
By engaging communities in neuropathic pain prevention and awareness, we can help reduce the burden of this condition and improve the lives of those affected. |
7. Future Directions in Neuropathic Pain Research
As our understanding of neuropathic pain continues to evolve, so does the landscape of research and treatment options. Here are some of the most promising areas of focus for the future of neuropathic pain management:
Advancements in Understanding Neuropathic Pain Mechanisms
One key area of ongoing research is the investigation of the complex mechanisms underlying the development and maintenance of neuropathic pain. This includes studying the roles of:
- Ion channels: Researchers are exploring the involvement of specific ion channels, such as sodium, calcium, and potassium channels, in the generation and propagation of neuropathic pain signals[26].
- Neurotransmitters and receptors: Investigating the alterations in neurotransmitter systems, such as glutamate, GABA, and serotonin, and their receptors can provide insights into the modulation of neuropathic pain[27].
- Glial cells: Studying the activation and contribution of glial cells, such as microglia and astrocytes, to the inflammatory and neuropathic pain processes can help identify new therapeutic targets[28].
- Epigenetic factors: Examining the role of epigenetic modifications, such as DNA methylation and histone acetylation, in the regulation of pain-related gene expression can shed light on the development and persistence of neuropathic pain[25].
By deepening our understanding of these mechanisms, researchers can identify novel targets for prevention, diagnosis, and treatment of neuropathic pain.
Studying changes in neurotransmitters and their receptors can provide insights into neuropathic pain modulation.
Novel Therapeutic Targets and Drug Development
As our knowledge of neuropathic pain mechanisms expands, so does the potential for developing new and more targeted therapies. Some promising areas of drug development include:
- Ion channel modulators: Developing compounds that selectively target and modulate specific ion channels involved in neuropathic pain, such as Nav1.7 or Cav2.2, can provide more precise and effective pain relief[26].
- Neurotransmitter receptor ligands: Designing drugs that bind to and modulate specific neurotransmitter receptors, such as NMDA or GABA receptors, can help regulate pain signaling and reduce neuropathic pain[27].
- Glial cell modulators: Targeting the activation and function of glial cells, such as microglia or astrocytes, with specific compounds can help reduce neuroinflammation and neuropathic pain[28].
- Epigenetic modulators: Developing drugs that target epigenetic mechanisms, such as histone deacetylase inhibitors or DNA methyltransferase inhibitors, can help regulate the expression of pain-related genes and reduce neuropathic pain[25].
By expanding the arsenal of therapeutic options, we can provide more personalized and effective treatments for patients with neuropathic pain.
Potential of Cold Plasma Therapy in Neuropathic Pain Management
Cold plasma therapy, particularly Mirari Cold Plasma and its focus on nitric oxide (NO), represents a promising frontier in neuropathic pain management. As research continues to elucidate the mechanisms by which NO modulates pain signaling, inflammation, and nerve repair, cold plasma therapy may emerge as a valuable adjunct or alternative to traditional treatments[18].
Future studies may explore:
- Optimal treatment parameters and protocols for various types and stages of neuropathic pain[18].
- Long-term efficacy and safety of cold plasma therapy compared to conventional pharmacological and non-pharmacological approaches[18].
- Potential synergistic effects of combining cold plasma therapy with other emerging or established treatments, such as ion channel modulators or neurotransmitter receptor ligands[18].
- Applications of cold plasma therapy in preventing or reversing the progression of neuropathic pain in at-risk populations[18].
As evidence accumulates, cold plasma therapy may become an increasingly important tool in the multimodal management of neuropathic pain, offering patients a safe, non-invasive, and targeted treatment option[18].
Cold plasma therapy shows promise for neuropathic pain, with future research needed on its optimal use, efficacy, and potential synergies.
Personalized Medicine Approaches
Another promising area of research is the development of personalized medicine approaches to neuropathic pain management. This involves tailoring treatment strategies to an individual patient’s unique genetic, molecular, and clinical profile.
- Pharmacogenomics: Studying the influence of genetic variations on an individual’s response to pain medications can help predict the efficacy and side effects of specific drugs and guide personalized treatment selection[1].
- Biomarker identification: Identifying specific biomarkers, such as gene expression profiles, protein levels, or neuroimaging patterns, that can predict the development, severity, or treatment response of neuropathic pain can help stratify patients and optimize individualized care[1].
- Precision diagnostics: Developing advanced diagnostic tools, such as high-resolution neuroimaging or sensory phenotyping, can help accurately characterize the specific type and mechanisms of neuropathic pain in individual patients and guide targeted treatment approaches[1].
- Personalized non-pharmacological interventions: Tailoring non-pharmacological approaches, such as neuromodulation parameters or psychological therapies, to an individual’s specific needs and preferences can enhance the effectiveness and adherence to these treatments[1].
By moving towards a more personalized approach to neuropathic pain management, we can optimize treatment outcomes, minimize side effects, and improve the quality of life for patients with this challenging condition[1].
Strategies for Early Detection and Intervention
Finally, future research efforts will likely focus on developing strategies for the early detection and intervention of neuropathic pain. This may involve:
- Predictive modeling: Developing and validating predictive models that integrate genetic, clinical, and environmental risk factors to identify individuals at high risk for developing neuropathic pain[19].
- Screening tools: Creating and implementing simple, non-invasive screening tools, such as questionnaires or sensory tests, that can detect early signs of neuropathic pain in at-risk populations, such as those with diabetes or chemotherapy exposure[19].
- Preventive interventions: Evaluating the effectiveness of preventive interventions, such as tight glycemic control, vitamin supplementation, or neuroprotective agents, in reducing the incidence or severity of neuropathic pain in high-risk groups[19].
- Early treatment initiation: Studying the impact of early initiation of pharmacological and non-pharmacological treatments on the course and outcomes of neuropathic pain, and developing guidelines for timely intervention based on risk profiles and early signs[19].
By shifting the focus towards early detection and intervention, we may be able to prevent or mitigate the development of chronic, debilitating neuropathic pain and improve the long-term outcomes for patients at risk[19].

Future research will aim at early detection and intervention for neuropathic pain through predictive models, screening tools, and preventive measures.
8. Takeaways
- Neuropathic pain is a complex, chronic pain condition caused by damage or dysfunction of the somatosensory nervous system, characterized by distinct symptoms such as burning, shooting pain, allodynia, and hyperalgesia[1].
- Multiple factors can contribute to the development of neuropathic pain, including diabetes, chemotherapy, nerve injury, autoimmune disorders, and genetic predisposition[29].
- Diagnosis of neuropathic pain involves a comprehensive clinical assessment, including history, physical examination, and diagnostic tests such as neuroimaging, neurophysiology, and quantitative sensory testing[30].
- Management of neuropathic pain typically involves a multimodal approach, combining pharmacological treatments (e.g., antidepressants, anticonvulsants, topical agents), non-pharmacological interventions (e.g., physical therapy, psychological therapies, complementary and alternative medicine), and advanced interventional procedures (e.g., nerve blocks, spinal cord stimulation) as needed[29].
- Cold plasma therapy, particularly Mirari Cold Plasma and its focus on nitric oxide (NO), represents a promising emerging treatment option for neuropathic pain, offering a safe, non-invasive, and targeted approach to pain relief and nerve repair[31].
- Effective management of neuropathic pain also involves patient education, self-management strategies, and ongoing monitoring and adjustment of treatment plans to optimize outcomes and quality of life[23].
- Prevention of neuropathic pain involves a combination of lifestyle modifications, regular health screenings, effective management of underlying conditions, patient education, and community awareness and support programs[2].
- Future research directions in neuropathic pain include advancing our understanding of pain mechanisms, developing novel therapeutic targets and personalized treatment approaches, and implementing strategies for early detection and intervention[26].
In conclusion, neuropathic pain is a complex, often debilitating condition that requires a comprehensive, multidisciplinary approach to management. By staying at the forefront of research and treatment advances, such as the emerging field of cold plasma therapy with Mirari Cold Plasma, healthcare providers can offer patients new hope for relief and improved quality of life.
As we continue to unravel the intricacies of neuropathic pain and develop more targeted, personalized therapies, it is crucial to empower patients with the knowledge and tools they need to take an active role in their care. This includes education about risk factors, lifestyle modifications, and self-management strategies, as well as access to support services and resources.
Ultimately, the future of neuropathic pain management lies in a collaborative, patient-centered approach that integrates cutting-edge science, compassionate care, and a commitment to improving outcomes for the millions of individuals affected by this challenging condition. By working together, researchers, clinicians, and patients can chart a path towards a world where neuropathic pain is effectively prevented, treated, and overcome.
9. FAQs
What are the most common symptoms of neuropathic pain?
The most common symptoms of neuropathic pain include burning, shooting, or electric-like pain; tingling or “pins and needles” sensations; numbness or reduced sensation in the affected area; and increased sensitivity to touch or temperature. These symptoms may be constant or intermittent and can significantly impact daily functioning and quality of life[1].
How is neuropathic pain diagnosed?
Neuropathic pain is diagnosed through a comprehensive clinical assessment, which includes a detailed history of symptoms, medical conditions, and medications; a thorough physical and neurological examination; and diagnostic tests such as neuroimaging (e.g., MRI, CT), neurophysiology (e.g., nerve conduction studies, electromyography), and quantitative sensory testing. The specific diagnostic approach may vary depending on the suspected underlying cause and the pattern of symptoms[30].
What are the first-line treatments for neuropathic pain?
The first-line treatments for neuropathic pain typically include antidepressants (e.g., tricyclic antidepressants, serotonin-norepinephrine reuptake inhibitors) and anticonvulsants (e.g., gabapentin, pregabalin). These medications work by modulating pain signaling in the nervous system and can provide significant relief for many patients. Other options, such as topical agents (e.g., lidocaine, capsaicin) or low-dose opioids, may be considered depending on the individual case[29].
How can cold plasma therapy, like Mirari Cold Plasma, help with neuropathic pain?
Mirari Cold Plasma, developed by General Vibronics, is a cutting-edge treatment that harnesses the power of nitric oxide (NO) to provide targeted relief for neuropathic pain. By delivering precise, controlled doses of NO to the affected area, cold plasma therapy can help modulate pain signaling, reduce inflammation, improve blood flow and oxygenation to the nerves, and stimulate nerve repair. This safe, non-invasive approach offers a promising alternative or adjunct to traditional pharmacological treatments, without the risk of systemic side effects[31].
What lifestyle changes can help prevent or manage neuropathic pain?
Several lifestyle modifications can help prevent or manage neuropathic pain, including: maintaining a healthy weight through a balanced diet and regular exercise; avoiding smoking and excessive alcohol consumption; managing stress through relaxation techniques or mindfulness practices; ensuring adequate sleep; and protecting against nerve injuries by using proper body mechanics and ergonomics. For those with underlying conditions that can lead to neuropathic pain, such as diabetes, strict adherence to treatment plans and regular monitoring are crucial for preventing nerve damage[2].
10. References
- Cleveland Clinic. (2023). Neuropathic Pain (Nerve Pain): What It Is, Causes & Symptoms. https://my.clevelandclinic.org/health/diseases/15833-neuropathic-pain
- Healthline. (2024). Neuropathic Pain: Causes, Symptoms, and Treatment. https://www.healthline.com/health/neuropathic-pain
- Wikipedia. (2024). Neuropathic pain. https://en.wikipedia.org/wiki/Neuropathic_pain
- WebMD. (2024). Neuropathic Pain Causes, Treatment, and Medication. https://www.webmd.com/pain-management/neuropathic-pain
- Healthdirect. (2024). Nerve pain (neuralgia) – causes, diagnosis and treatments. https://www.healthdirect.gov.au/nerve-pain
- NCBI. (2018). Genetic studies of human neuropathic pain conditions: a review. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5828382/
- BMJ. (2009). Diagnosis and management of neuropathic pain. https://doi.org/10.1136/bmj.b3002
- Mayo Clinic. (2024). Peripheral neuropathy – Symptoms and causes. https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/symptoms-causes/syc-20352061
- WebMD. (2024). Nerve Pain (Neuropathic Pain): Symptoms, Causes, & Treatment. https://www.webmd.com/pain-management/ss/slideshow-neuropathy
- PubMed. (2024). Antidepressants in the treatment of neuropathic pain. https://pubmed.ncbi.nlm.nih.gov/15910402/
- PubMed Central. (2024). The neuropathic pain: An overview of the current treatment. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6431761/
- PubMed. (2024). Anticonvulsants for neuropathic pain syndromes. https://pubmed.ncbi.nlm.nih.gov/11129121/
- PubMed Central. (2024). The neuropathic pain: An overview of the current treatment and management. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6431761/
- PubMed. (2024). Topical Treatment of Peripheral Neuropathic Pain. https://pubmed.ncbi.nlm.nih.gov/28042075/
- Hearn, L., & de C Williams, A. C. (2015). Psychological therapies for the management of chronic neuropathic pain in adults. Cochrane Database of Systematic Reviews. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6485637/
- Physiopedia. (2024). Neuropathic Pain. https://www.physio-pedia.com/Neuropathic_Pain
- Spine-health. (2024). Additional Treatments for Neuropathic Pain. https://www.spine-health.com/treatment/pain-management/additional-treatments-neuropathic-pain
- NCBI. (2024). Beneficial effects of cold atmospheric plasma on inflammatory phase. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7843664/
- Varshney, V., Osborn, J., Chaturvedi, R., & Shah, V. (2021). Advances in the interventional management of neuropathic pain. Pain Management. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7867895/
- Deer, T. R., Mekhail, N., Provenzano, D., Pope, J. E., Krames, E. S., Leong, M., Levy, R. M., Abejon, D., Buchser, E., Burton, A. W., Caraway, D., Cousins, M., De Andrés, J., Diwan, S., Eldabe, S., Foreman, R. D., Grigsby, E. J., Huygen, F. J., Jacobs, M. S., … & Wallace, M. (2019). Spinal Cord Stimulation for Neuropathic Pain: Current Trends and Future Applications. Pain Medicine. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6119923/
- Caragher, S. P., Khouri, K. S., Raasveld, F. V., Winograd, J. M., Valerio, I. L., Gfrerer, L., & Eberlin, K. R. (2022). The Peripheral Nerve Surgeon’s Role in the Management of Neuropathic Pain. Plastic and Reconstructive Surgery. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10287132/
- Mehringer Chiropractic. (2024). Managing Neuropathic Pain: Lifestyle Changes and Coping Strategies. https://www.mehringerchiropractic.com/managing-neuropathic-pain-lifestyle-changes-and-coping-strategies/
- WinSanTor. (2024). Five Lifestyle Changes for Peripheral Neuropathy. http://winsantor.com/five-lifestyle-changes-to-relieve-symptoms-for-peripheral-neuropathy/
- Foundation for Peripheral Neuropathy. (2024). The Foundation For Peripheral Neuropathy. https://www.foundationforpn.org
- PubMed. (2024). Non pharmacologic treatment of neuropathic pain. https://pubmed.ncbi.nlm.nih.gov/18191370/
- Petroianu, G. A., Aloum, L., & Adem, A. (2023). Neuropathic pain: Mechanisms and therapeutic strategies. Frontiers in Cell and Developmental Biology. https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2023.1072629/full
- Cavalli, E., Mammana, S., Nicoletti, F., Bramanti, P., & Mazzon, E. (2024). The neuropathic pain: An overview of the current treatment and future therapeutic approaches. I.R.C.C.S. Centro Neurolesi Bonino Pulejo. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6431761/
- NPS MedicineWise. (2024). About neuropathic pain. NPS MedicineWise. https://www.nps.org.au/professionals/neuropathic-pain
- Schlereth, T. (2019). Guideline “diagnosis and non interventional therapy of neuropathic pain” of the German Society of Neurology. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7650069/
- NICE. (2020). Neuropathic pain in adults: pharmacological management in non-specialist settings. https://www.nice.org.uk/guidance/cg173
- Mirari Doctor. (2024). Mirari Doctor Introduces Revolutionary Cold Plasma Technology for Skin Rejuvenation and Wound Healing. https://markets.businessinsider.com/news/stocks/mirari-doctor-introduces-revolutionary-cold-plasma-technology-for-skin-rejuvenation-and-wound-healing-1033225816
Related articles
Made in USA