Cold plasma for diabetes represents a groundbreaking advancement in medical technology, offering new hope for patients struggling with diabetic complications, particularly chronic wounds and foot ulcers. This innovative therapy harnesses the power of ionized gas at room temperature to accelerate healing, reduce infection, and improve overall diabetes management outcomes without the risks associated with traditional thermal treatments.
Unlike conventional diabetes treatments that often focus solely on blood sugar control, cold atmospheric plasma (CAP) therapy addresses the complex cascade of complications that arise from prolonged hyperglycemia. The technology generates reactive oxygen and nitrogen species that stimulate cellular repair mechanisms while providing powerful antimicrobial effects against resistant bacterial strains commonly found in diabetic wounds.
Understanding Cold Plasma Technology for Diabetes Management
Scientific Mechanisms Behind Cold Plasma Therapy
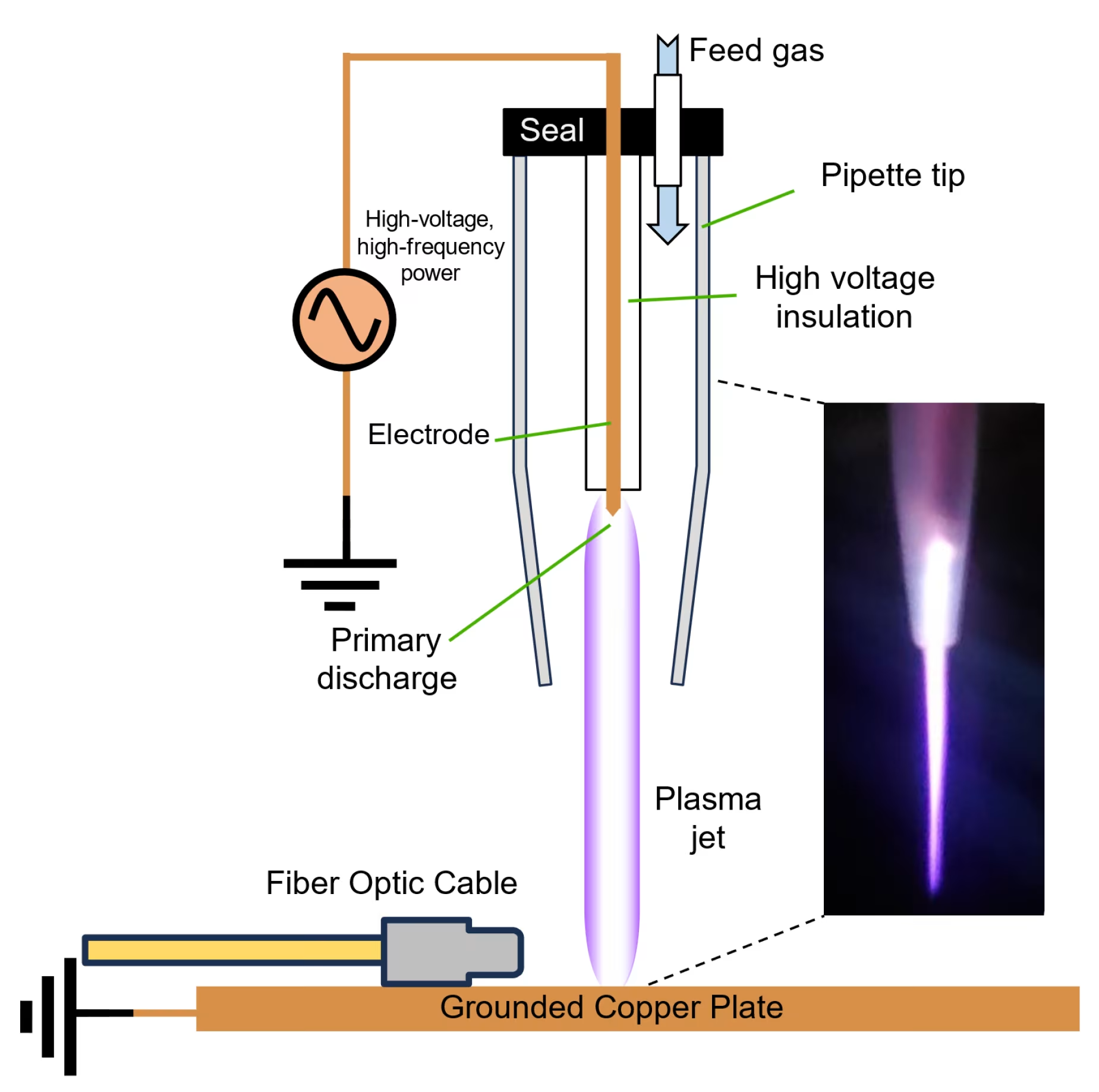
Cold atmospheric plasma operates through multiple interconnected biological pathways that directly address the underlying complications of diabetes. The technology creates a controlled environment of reactive species, including nitric oxide (NO), reactive oxygen species (ROS), and reactive nitrogen species (RNS), which interact with biological tissues to promote healing and reduce inflammation[1].
When applied to diabetic tissues, cold plasma generates physiologically relevant concentrations of these bioactive molecules. Research demonstrates that CAP treatment significantly increases the activity of antioxidant enzymes including catalase, superoxide dismutase, and glutathione peroxidase in diabetic patients[2]. This enhanced antioxidant capacity helps combat the oxidative stress that characterizes diabetes and contributes to its complications.
Nitric Oxide Production and Diabetic Healing
One of the most significant mechanisms involves the controlled production of nitric oxide, which plays crucial roles in diabetic wound healing. Cold plasma treatment increases endothelial nitric oxide synthase (eNOS) expression, leading to enhanced NO production that affects vascular function and tissue repair processes[3].
The Mirari Cold Plasma System, developed by General Vibronics and commercialized by Mirari Doctor, utilizes proprietary nitric oxide-based technology that distinguishes it from traditional ROS-based systems. This approach provides enhanced safety profiles while maintaining therapeutic efficacy for diabetic applications, particularly in wound care and circulation improvement.
Addressing Diabetic Complications Through Plasma Therapy
Cold plasma therapy targets multiple pathophysiological processes that contribute to diabetic complications. The technology has been shown to reduce advanced glycation end products (AGEs), which accumulate in diabetic patients and contribute to tissue damage[4]. Additionally, CAP treatment helps normalize inflammatory cytokine levels, reducing the chronic inflammation that characterizes diabetes.
Studies indicate that cold plasma treatment can significantly reduce oxidative stress markers including malondialdehyde (MDA), advanced oxidation protein products (AOPP), and oxidized low-density lipoprotein (oxLDL) in diabetic patients[1]. This reduction in oxidative burden helps protect tissues from further damage while promoting repair mechanisms.
Clinical Applications of Cold Plasma for Diabetes
Diabetic Foot Ulcer Treatment
Diabetic foot ulcers represent one of the most challenging complications of diabetes, affecting millions of patients worldwide and often leading to amputation when conventional treatments fail. Cold plasma therapy has emerged as a highly effective treatment option for these difficult-to-heal wounds.
A landmark randomized clinical trial involving 43 patients with 62 diabetic foot ulcers demonstrated that cold plasma therapy significantly accelerated wound healing compared to standard care[5]. The study found that CAP treatment resulted in greater wound surface area reduction and faster time to clinically meaningful wound improvement.
Antimicrobial Effects in Diabetic Wounds
One of the most significant advantages of cold plasma therapy for diabetic foot ulcers is its powerful antimicrobial activity. Research shows that CAP treatment effectively reduces bacterial load, particularly Staphylococcus aureus, which is commonly found in diabetic wound infections[6]. This antimicrobial effect occurs immediately after treatment and helps prevent the progression to serious infections that could require amputation.
Clinical studies have demonstrated that cold plasma treatment is safe for diabetic foot ulcers, with no serious adverse device effects reported in controlled trials[6]. More than half of the wounds treated showed greater than 50% size reduction during two weeks of treatment, with some wounds healing completely during this period.
Systemic Diabetes Management Benefits
Beyond wound healing, cold plasma therapy shows promise for systemic diabetes management. Animal studies have demonstrated that CAP treatment can help regulate blood glucose levels in diabetic subjects[4]. The therapy appears to work by reducing oxidative stress and inflammation, which are key contributors to insulin resistance and diabetic complications.
Research indicates that cold plasma treatment can improve the function of glycated proteins and enzymes that become damaged in diabetes[2]. This restoration of protein function may help improve overall metabolic control and reduce the risk of long-term complications.
Technical Specifications of Cold Plasma Diabetes Treatment
| Parameter | Specification | Clinical Application |
|---|---|---|
| Operating Temperature | Room temperature (20-25°C) | Safe for diabetic skin and compromised circulation |
| Treatment Duration | 10-15 minutes per session | Optimal exposure for diabetic wound healing |
| Session Frequency | Daily to 3x weekly | Customizable based on wound severity |
| Reactive Species | NO, ROS, RNS production | Multiple therapeutic mechanisms |
| Antimicrobial Activity | Broad-spectrum pathogen reduction | Effective against resistant bacteria |
| Penetration Depth | 2-5mm tissue penetration | Reaches diabetic wound bed effectively |
Clinical Benefits and Treatment Outcomes
| Diabetic Condition | Treatment Protocol | Reported Outcomes | Timeline |
|---|---|---|---|
| Diabetic Foot Ulcers | Daily treatment for 2 weeks | 43% average wound reduction | 2-4 weeks |
| Chronic Wounds | 3x weekly for 3 weeks | Accelerated granulation tissue formation | 3-6 weeks |
| Infection Control | Daily until infection clears | Immediate bacterial load reduction | 24-48 hours |
| Circulation Enhancement | 2x weekly maintenance | Improved tissue oxygenation | 1-2 weeks |
| Oxidative Stress | Weekly treatments | Reduced inflammatory markers | 4-8 weeks |
| Wound Pain | As needed for comfort | Significant pain reduction | Immediate |
Real-World Clinical Outcomes
Clinical experience with cold plasma therapy for diabetes has yielded impressive results across multiple healthcare settings. In a comprehensive study of diabetic foot ulcers, patients receiving CAP treatment showed significantly better healing outcomes compared to standard care alone[7]. The treatment was particularly effective in patients with treatment-resistant wounds that had failed to respond to conventional therapies.
Healthcare providers report that cold plasma therapy offers several advantages over traditional diabetic wound treatments. The non-invasive nature of the therapy eliminates risks associated with surgical debridement, while the antimicrobial effects reduce the need for systemic antibiotics that may have adverse effects in diabetic patients.
Long-Term Benefits for Diabetic Patients
Beyond immediate wound healing benefits, cold plasma therapy may provide long-term advantages for diabetic patients. The technology’s ability to improve antioxidant enzyme function and reduce oxidative stress could help prevent future complications[2]. Additionally, the enhanced healing capacity observed with CAP treatment may reduce the risk of recurrent ulceration and amputation.
Studies suggest that regular cold plasma treatment may help maintain better tissue health in diabetic patients, potentially reducing the overall burden of diabetic complications. The therapy’s ability to improve microcirculation and reduce inflammation could have systemic benefits beyond the treated area.
Safety Profile and Patient Experience
Excellent Safety Record in Diabetic Patients
Cold plasma therapy demonstrates an outstanding safety profile in diabetic patients, who often have compromised healing and increased infection risk. Clinical trials consistently report minimal adverse effects, with most patients experiencing no discomfort during treatment[8].
In a comprehensive safety study involving diabetic foot ulcer patients, researchers found that 56.9% of treatment sessions caused no pain, while 40.1% resulted in only mild discomfort[8]. No serious adverse device effects were reported, and the few side effects that occurred were mild and temporary.
Patient Tolerance and Comfort
The non-thermal nature of cold plasma therapy makes it particularly suitable for diabetic patients who may have reduced sensation due to neuropathy. Unlike thermal treatments that could cause burns in patients with impaired sensation, cold plasma operates at room temperature, eliminating this risk.
Patients typically describe the treatment sensation as a mild tingling or slight warmth. The therapy can be administered in outpatient settings without the need for anesthesia or special preparation, making it accessible for patients with mobility limitations or other diabetic complications.
Comparing Cold Plasma to Traditional Diabetes Treatments
Advantages Over Conventional Wound Care
Cold plasma therapy offers several distinct advantages over traditional diabetic wound care approaches. Unlike debridement procedures that can be painful and may remove healthy tissue along with damaged areas, cold plasma selectively targets pathological processes while preserving healthy tissue.
The technology’s antimicrobial effects are particularly valuable in diabetic wound care, where infection control is crucial. Traditional antibiotic treatments may be less effective due to poor circulation in diabetic patients and the presence of biofilms that protect bacteria from antimicrobial agents. Cold plasma can penetrate biofilms and eliminate bacteria without promoting antibiotic resistance.
Cost-Effectiveness and Healthcare Outcomes
From a healthcare economics perspective, cold plasma therapy may offer significant cost savings by reducing the need for more expensive interventions. By accelerating wound healing and preventing infections, CAP treatment can help patients avoid hospitalizations, surgical procedures, and amputations that carry substantial costs and morbidity.
The Mirari Cold Plasma System’s portability and ease of use make it particularly valuable for diabetes care, as it can be used in various healthcare settings without requiring specialized facilities or extensive training. This accessibility could help expand treatment options for diabetic patients in underserved areas.
Future Directions and Research Developments
Emerging Applications in Diabetes Care
Research into cold plasma applications for diabetes continues to expand beyond wound healing. Current investigations include the technology’s potential for improving insulin sensitivity, reducing diabetic neuropathy symptoms, and preventing diabetic complications through regular maintenance treatments.
Scientists are exploring the use of cold plasma therapy as an adjunctive treatment for diabetic retinopathy and nephropathy, two serious complications that can lead to blindness and kidney failure. The technology’s anti-inflammatory and antioxidant effects may help protect these vulnerable tissues from diabetic damage.
Integration with Comprehensive Diabetes Management
Future developments may include integration of cold plasma therapy with other diabetes management technologies, such as continuous glucose monitoring and insulin delivery systems. This comprehensive approach could provide personalized treatment protocols that optimize both metabolic control and complication prevention.
The growing body of research supporting cold plasma therapy for diabetes has attracted attention from healthcare providers and patients seeking alternatives to conventional treatments. As more clinical data becomes available, the technology is likely to play an increasingly important role in comprehensive diabetes care.
Patient-Focused Frequently Asked Questions
Is cold plasma therapy safe for all diabetic patients?
Cold plasma therapy has an excellent safety profile for most diabetic patients, including those with compromised circulation and neuropathy. Clinical studies consistently show minimal adverse effects, with most patients experiencing no discomfort during treatment. However, patients with active infections at the treatment site, certain medical implants, or severe cardiovascular conditions should be evaluated carefully before treatment. Healthcare providers will assess individual suitability and monitor patients throughout the treatment course to ensure safety and effectiveness.
How quickly can diabetic patients see results from cold plasma treatment?
Most diabetic patients begin to notice improvements in wound healing within the first week of cold plasma treatment. For diabetic foot ulcers, significant wound size reduction typically becomes apparent within 2-4 weeks of consistent treatment. The antimicrobial effects are often immediate, with bacterial load reduction observable within 24-48 hours. However, the timeline varies based on wound severity, overall health status, and blood sugar control. Patients with better diabetes management generally experience faster healing responses.
Can cold plasma therapy replace traditional diabetes medications?
Cold plasma therapy is designed to complement, not replace, traditional diabetes medications and management strategies. While research shows that CAP treatment can help improve blood sugar control and reduce oxidative stress, it should be used as part of a comprehensive diabetes management plan that includes appropriate medications, diet, exercise, and regular monitoring. Patients should never discontinue prescribed diabetes medications without consulting their healthcare provider, as this could lead to dangerous blood sugar fluctuations.
How does cold plasma treatment compare to other diabetic wound therapies?
Cold plasma therapy offers several advantages over traditional diabetic wound treatments. Unlike surgical debridement, which can be painful and may remove healthy tissue, cold plasma selectively targets damaged areas while preserving healthy tissue. Compared to antibiotic treatments, CAP provides immediate antimicrobial effects without promoting bacterial resistance. The therapy also stimulates natural healing processes more effectively than passive wound dressings, often leading to faster closure times and better tissue quality in the healed wound.
What should diabetic patients expect during cold plasma treatment sessions?
During cold plasma treatment, diabetic patients typically experience a mild tingling sensation or slight warmth at the treatment site. Sessions usually last 10-15 minutes and can be performed in outpatient settings without special preparation. Most patients find the treatment comfortable and relaxing. Some may notice a faint blue glow from the plasma device, which is normal and indicates proper operation. After treatment, patients can immediately resume normal activities, though they should follow any specific wound care instructions provided by their healthcare team.
Medical Disclaimer: This information is for educational purposes only and should not replace professional medical advice. Diabetic patients should always consult with qualified healthcare providers before starting any new treatment. Individual responses to cold plasma therapy may vary, and treatment decisions should be based on comprehensive medical evaluation and ongoing diabetes management needs.
References
- Nature. (2019). The effect of cold atmospheric plasma on diabetes-induced enzyme dysfunction. https://www.nature.com/articles/s41598-019-56459-y
- Functional Foods in Health and Disease. (2021). The effect of cold plasma on antioxidant enzymes, minerals, and some of the levels of the biochemical parameters in the subjects with type 2 diabetes mellitus samples. https://ffhdj.com/index.php/BioactiveCompounds/article/view/783
- Biomedicine \& Pharmacotherapy. (2023). Cold atmospheric plasma induces the curing mechanism of diabetic wounds by regulating the oxidative stress mediators iNOS and NO. https://pubmed.ncbi.nlm.nih.gov/38000357/
- Plasma Medicine. (2021). Cold Atmospheric Plasma Treatment: A Novel Method of Diabetes Therapy. https://www.dl.begellhouse.com/journals/5a5b4a3d419387fb,734a683b298a445e,4241ccc03d750c8d.html
- JAMA Network Open. (2020). Effect of Cold Atmospheric Plasma Therapy vs Standard Therapy Placebo on Wound Healing in Patients With Diabetic Foot Ulcers. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2768340
- Journal of Wound Care. (2023). Cold plasma treatment is safe for diabetic foot ulcers and decreases Staphylococcus aureus bacterial load. https://pubmed.ncbi.nlm.nih.gov/37029969/
- Frontiers in Medicine. (2025). Advancing chronic and acute wound healing with cold atmospheric plasma. https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1527736/full
- Vietnam Medical Journal. (2023). Investigating Adverse Effects of Cold Plasma in Treating Second and Third Degree Burns. https://tapchiyhocvietnam.vn/index.php/vmj/article/download/5055/4625
Related articles
Made in USA