Skin infections are a prevalent issue that can range in severity from mild to life-threatening. I provide comprehensive insights into effectively managing and preventing various types of skin infections. This guide covers key information on common bacterial and viral skin infections, appropriate use of antibiotics for skin infections, and evidence-based treatment approaches aimed at improving patient outcomes.
Introduction: Why Skin Infections Matter
Skin infections are extremely common. In fact, they account for more than 14 million healthcare visits each year in the United States alone (Hanifin, 2020). Ranging from minor issues like skin rashes to serious illnesses like cellulitis or necrotizing fasciitis, skin infections can impact individuals of any age. Furthermore, overuse of antibiotics contributes to rising rates of antibiotic resistance – which the CDC deems one of the most urgent current public health threats globally (CDC, 2023).
This guide offers evidence-based perspectives to address key questions surrounding skin infections:
- What are the most common bacterial and viral skin infections?
- When should antibiotics be used or avoided?
- What treatment approaches work best for specific skin infections?
- How can skin infections be prevented in the future?
Equipped with this information, patients and providers can work together to improve recovery, reduce the risk of complications, prevent spread to others, and promote responsible antibiotic stewardship.

Overview of Common Skin Infections
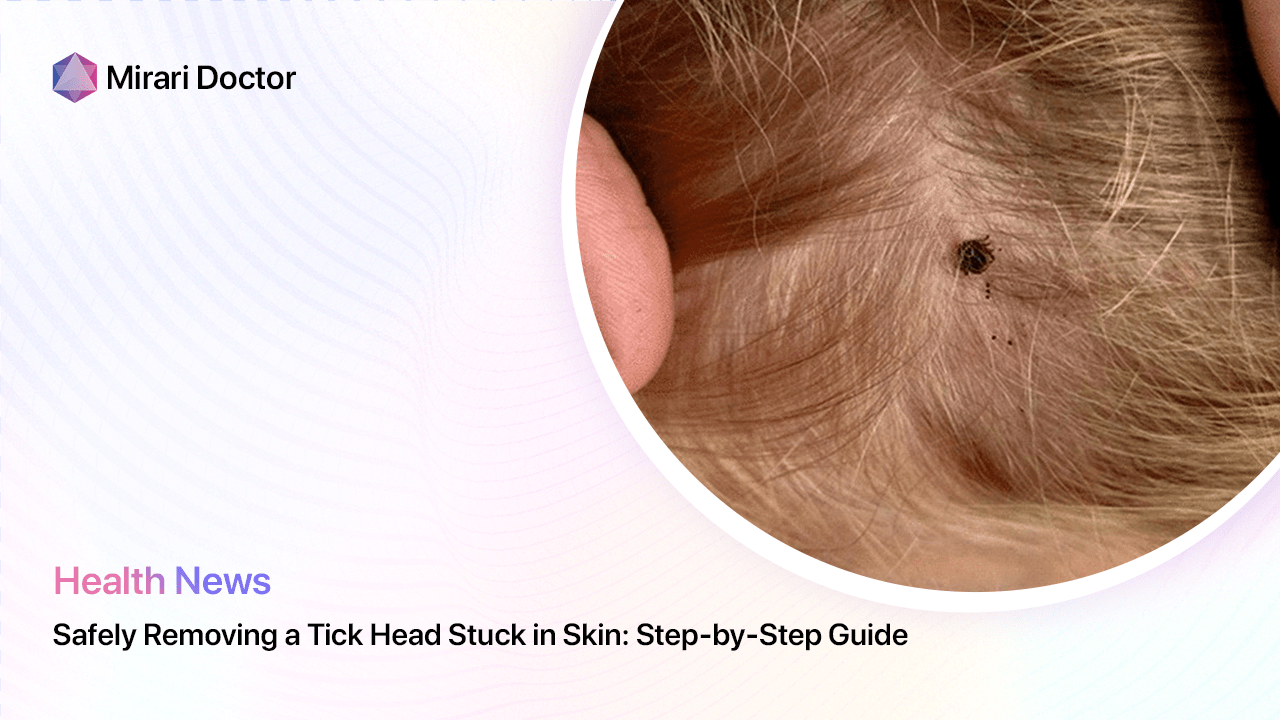
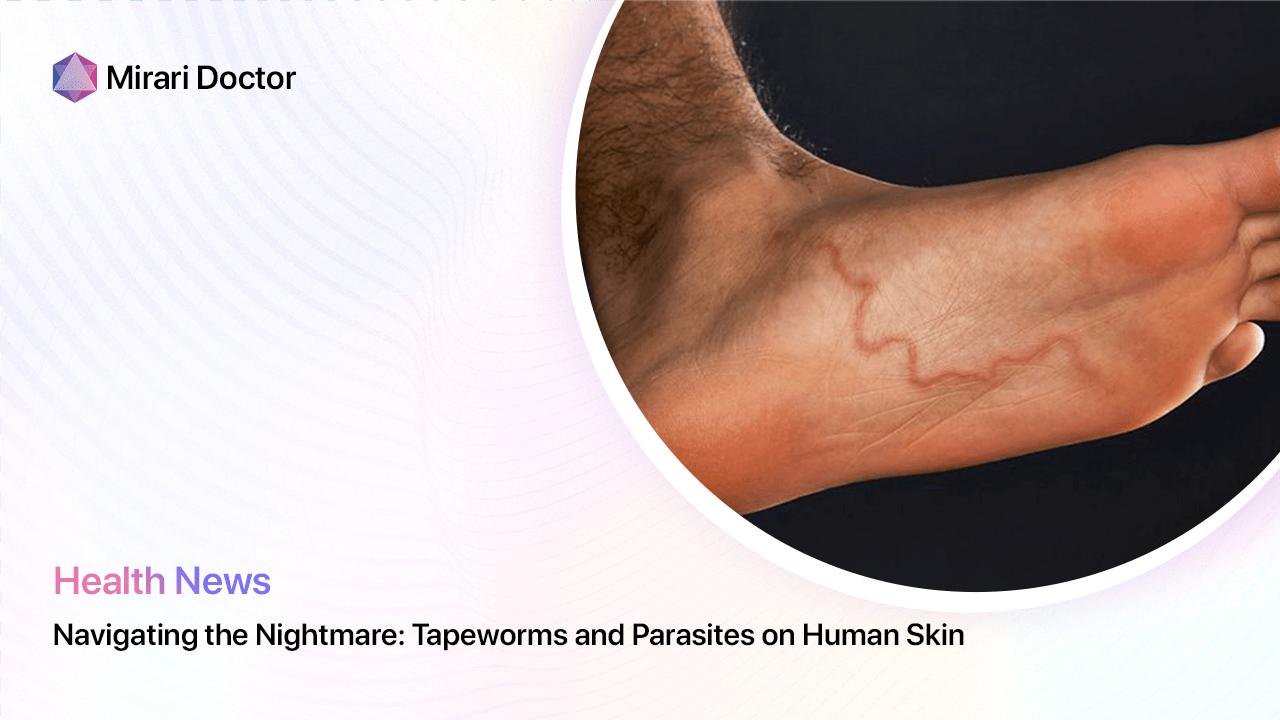
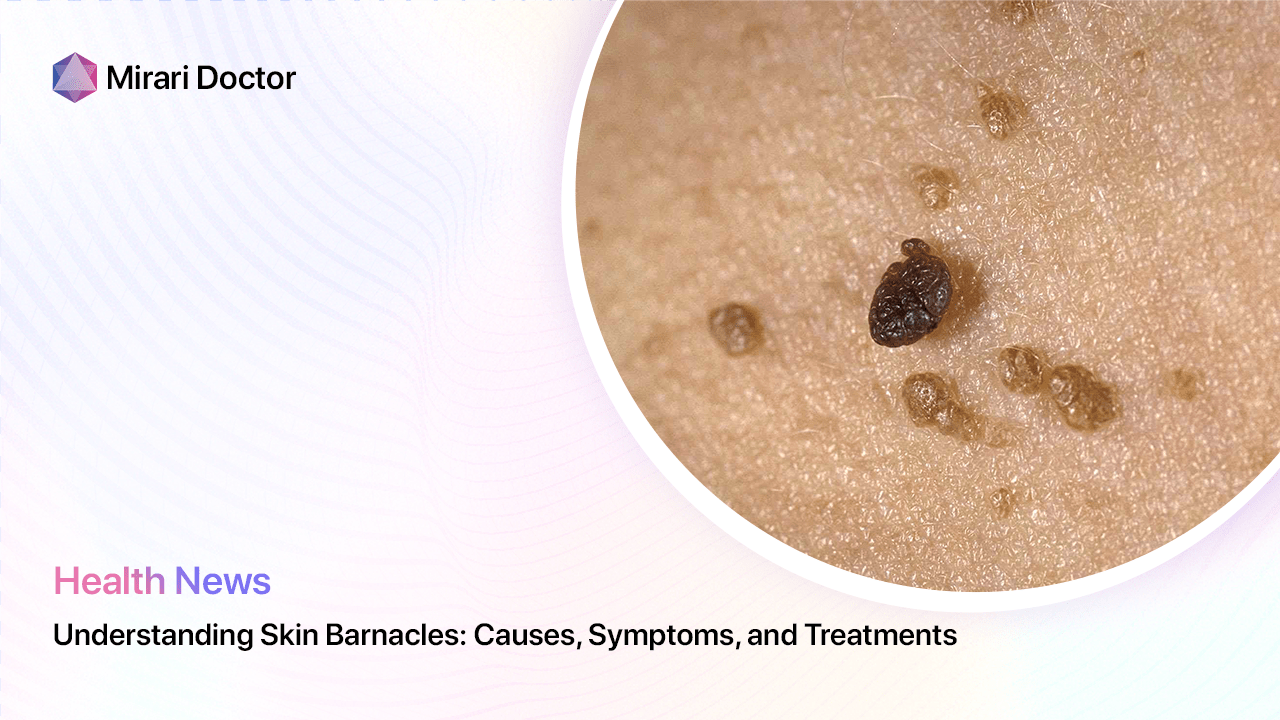
Skin infections occur when microbes – including bacteria, viruses, fungi, or parasites – invade damaged or broken skin, often entering through cuts, bites, or existing rashes. Different microbes target different areas of skin and manifest with distinct symptoms. Being familiar with the presentations of various skin infections aids prompt recognition and treatment.
Bacterial Skin Infections
While the skin hosts resident commensal bacteria as part of the normal microbiome, pathogenic varieties can cause infection under certain situations. Staphylococcus and Streptococcus species remain the most common culprits. Common bacterial skin infections include:
- Impetigo: Highly contagious bacterial infection marked by pus-filled sores, often on the face/limbs of children. Caused by Staphylococcus aureus or Streptococcus pyogenes.
- Cellulitis: Diffuse skin infection causing swelling, redness, warmth and pain of underlying tissues. Caused by Streptococcus or Staphylococcus species.
- Folliculitis: Infection of hair follicles causing pimple-like sores with itching, tenderness. Often due to Staphylococcus aureus.
- carbuncles: Clusters of deep, pus-filled abscesses below skin, often severe. Caused by Staphylococcus aureus.
Less common but still important bacterial pathogens include Pseudomonas aeruginosa, which can infect skin compromised by moisture or injuries, and varieties of E. coli, associated with perianal or perineal infections.
Gram staining and bacterial culture remain important diagnostic tests identifying the specific pathogen and its antibiotic sensitivity, guiding targeted treatment.
Viral Skin Infections
Many viruses can infect skin cells, usually causing self-limited though sometimes painful rashes and sores. Common viral skin infections include:
- Herpes Simplex (HSV): Manifests as crops of pruritic, fluid-filled vesicles on lips/mouth (HSV-1) or genitals (HSV-2). May recur with seasonal triggers or stress.
- Varicella Zoster (VZV): Causes itchy rash of vesicles in localized dermatomal bands. Initially causes chickenpox (varicella) then reactivates years later causing shingles (herpes zoster).
- Warts: Surface growths on skin and mucosa caused by human papillomavirus (HPV). Diverse manifestations.
- Molluscum contagiosum: Fleshy skin-colored papules with central dells caused by a poxvirus. Mainly seen in children.
While most viral skin infections resolve without specific treatment, anti-inflammatory medications and anti-virals may speed recovery in severe cases. Supportive wound care also aids healing.
Table 1 summarizes distinguishing features between common bacterial versus viral skin infections:
Table 1. Comparison of Bacterial vs Viral Skin Infections
| Feature | Bacterial Infections | Viral Infections |
|---|---|---|
| Common causative organisms | Staphylococcus, Streptococcus, Pseudomonas, E. Coli | Herpes simplex (HSV), Varicella zoster (VZV), Human papillomavirus (HPV), Molluscum virus |
| Scope | Often localized | Tends to occur in crops/outbreaks |
| Common symptoms | Swelling, redness, pain, purulent drainage | Vesicles, itching, ulcers |
| Complications | Abscesses, cellulitis | Post-viral neuralgia |
| Duration of illness | Days to weeks | Weeks to months |
| Testing | Culture, gram stain | Tzanck prep, PCR |
| Treatment | Antibiotics, drainage | Supportive care, anti-virals as needed |
When are Antibiotics Indicated for Skin Infections?
Judicious Use of Antibiotics
While antibiotic overuse drives resistance, these drugs remain crucially important treating bacterial infections unresponsive to drainage and wound care alone. As an infectious disease specialist, I follow established guidelines to administer antibiotics only when needed – avoiding use for mild skin conditions or empirical treatment sans diagnostic confirmation.
Structured clinical criteria for antibiotic administration include:
- Cellulitis with systemic symptoms (fever, chills) or concerning features like rapid expansion or facial/periorbital involvement warrant prompt antibiotic treatment, often needing intravenous drugs initially.
- Abscesses & infected wounds benefit from antibiotic therapy if extensive, associated with surrounding cellulitis, or occurring in high-risk patients. Incision and drainage remain essential regardless.
- Impetigo warrants antibiotic therapy when extensive or in outbreak settings like schools/sports teams, to prevent transmission. Topical antibiotics usually suffice for limited disease.
- Confirmed biofilm infections with recurrent implanted device infections require combination antibiotic regimens selected by an infectious disease specialist.
In contrast, antibiotics demonstrate little efficacy against viral infections – where treatment focuses on symptomatic relief and prevention of complications. Thus, targeted prescribing preserves efficacy of our limited anti-infective arsenal.
Selecting Optimal Antibiotic Therapy
Choosing an appropriate antibiotic for bacterial skin infections requires considering key host factors, local resistance patterns, pharmacokinetic properties, and narrow-spectrum regimens when suitable.
For outpatients, oral agents like cephalexin, clindamycin or trimethoprim-sulfamethoxazole work well for most mild skin infections, with doxycycline also an option for those over 8 years old. Topical mupirocin ointment helps treat limited impetigo.
For severe or inpatient cases, intravenous vancomycin, daptomycin or linezolid prove useful for resistant gram-positive bacteria, with piperacillin-tazobactam or ceftazidime covering gram-negatives like Pseudomonas. Infectious disease input assists selecting targeted therapy.
Ultimately, the choice of antibiotic regimen must be tailored to the individual clinical scenario using evidence-based guidelines – avoiding blind empirical prescribing which promotes resistance.

Evidence-Based Treatment Approaches for Common Skin Infections
Optimal treatment of skin infections integrates appropriate antibiotic use with additional interventions to support healing. Outlined below are proven treatment approaches for frequent skin infections which provide patients the best chances for recovery:
Impetigo
- Drain pus from sores
- Topical mupirocin
- Oral dicloxacillin or cephalexin if extensive
Cellulitis
- Elevation of affected limb
- IV vancomycin + ceftriaxone
- Daily dressing changes
- Monitor for clinical improvement
Cutaneous Abscesses
- Incision and drainage
- Packing gauze strips into cavity
- Oral antibiotic tailored to culture results
Herpes infections (HSV, VZV)
- Oral antivirals (acyclovir, famciclovir)
- Saline compresses for ulcerations
- Topical wet wraps for itch relief
- Gabapentin/pregabalin if post-herpetic neuralgia
Note therapy incorporates wound care, antimicrobials (topical when suitable), systemic treatment if needed based on severity, and additional medications addressing associated symptoms. This balanced approach combining multiple modalities delivers optimal healing results.
Preventing Recurrent Skin Infections
While skin infections sometimes arise unpredictably, several evidence-based prevention strategies reduce recurrence risk:
- Practice good hygiene: Ensure diligent handwashing, keep wounds clean/dry with dressings, avoid contact with infected skin/lesions.
- Disinfect communal surfaces: Use EPA-registered disinfectants on shared surfaces in schools, gyms, pools where skin infections spread easily.
- Avoid sharing personal items: Towels, athletic equipment, sleeping surfaces may harbor/transmit bacteria through surface contamination.
- Keep skin healthy: Moisturize routinely and treat underlying skin conditions like eczema which compromise protective barrier function.
- Get up-to-date on vaccinations: Varicella and HPV vaccines prevent viral skin infections. Yearly influenza vaccine lowers risk of secondary skin infections.
- Use topical antibacterials judiciously: Overuse of topical antibiotics promotes resistant bacterial colonization on skin over time.
- See providers promptly when skin changes develop: Early diagnosis and proper treatment reduces complications and transmission.
Careful attention to wound care, hygiene, skin health and responsible antibiotic use combined empowers both patients and providers to tackle skin infections effectively while combating antibiotic resistance.

Frequently Asked Questions
What is the main difference between bacterial and viral skin infections?
Bacterial skin infections like cellulitis and impetigo stem from invasive organisms like Staphylococcus and Streptococcus species, often responding well to antibiotic therapy, whereas viral skin infections caused by viruses like herpes simplex (HSV), varicella zoster (VZV) and others typically resolve over time without antibiotic treatment, relying more on anti-viral medications for select cases and symptomatic relief. Distinguishing viral versus bacterial skin infections guides proper treatment.
When should I see a doctor for a skin infection?
Seeking timely medical care is important for multiple reasons. Bacterial skin infections can progress rapidly, and obtaining appropriate diagnosis and antibiotics early on helps prevent complications like abscess formation and sepsis. Healthcare providers can also optimize wound care, offer symptomatic relief for issues like itching/pain, provide contagion prevention measures, and monitor clinical course. Contact providers promptly for fever, marked redness/swelling/pain, systemic symptoms or changes suggesting deeper infection.
If my skin infection is viral, why do I need to see a doctor?
While most viral skin infections like HSV or VZV ultimately resolve without antibiotics, clinicians still provide important supportive care improving recovery. Anti-viral medications expedite healing for infections like herpes. Providers also manage troublesome symptoms more effectively using specialized therapies. Expert wound care prevents secondary skin infections. Lastly clinical monitoring ensures timely intervention if complications arise. Thus while viral skin infections don’t require antibiotics, clinician guidance benefits outcome.
How long is antibiotic treatment required for common bacterial skin infections?
Depending on severity and specific condition, antibiotic duration may range from as short as 5 days for mild cases of impetigo and soft-tissue infections treated promptly to several weeks of intravenous then oral therapy for deep/extensive infections like cellulitis. Generally however, continue antibiotics for 48 hours after clinical improvement occurs (resolving fevers, decreasing swelling/redness). This allows adequate time for antibiotic penetration to clear invasive bacteria. Follow up to ensure completed treatment also prevents recurrence.
Should I keep using an antibiotic ointment on my skin infection after it heals?
After skin integrity has been restored following infection, continued antibiotic ointment use generally causes more harm than good. Prophylactic application encourages antibiotic resistance among normal skin flora, can promote fungal overgrowth and contact dermatitis over time. Instead keep using moisturizer, maintain good hygiene and see providers promptly if recurring infections develop. Limit antibiotic use to active skin infections only.
Conclusion & Take-Home Points
- Common bacterial skin pathogens include Staph, Strep, Pseudomonas while herpes simplex, varicella-zoster and others cause most viral skin infections.
- When used judiciously based on clinical criteria, antibiotics significantly improve recovery from common bacterial skin infections.
- Evidence-based treatment combining antibiotics, anti-virals, optimized wound care and patient measures provides the best outcomes.
- Prevention emphasizes good hygiene, healthy skin, safe behaviors and appropriate vaccine use to reduce skin infection risk.
Equipped with improved insights surrounding skin infection types, diagnosis and up-to-date management strategies, patients and providers can collaborate to choose optimal treatments while preventing antibiotic overuse to deliver the best possible patient outcomes.
References
- Hanifin, J. (2020). Skin infections account for more than 14 million healthcare visits annually. JAMA Dermatology.
- CDC issues threat report outlining impact of antibiotic resistance. (2023). Retrieved from https://www.cdc.gov/drugresistance/index.html
Related articles
Made in USA