As a medical professional, one of the most common questions I receive from patients who have undergone laparoscopic surgery is whether they can expect to develop acne or experience sudden breakouts during their recovery. While acne is not typically listed as a common side effect of laparoscopic procedures, some patients do report experiencing skin changes or flare-ups in the weeks following their surgery. In this comprehensive article, we’ll explore the potential links between laparoscopic surgery and acne, as well as strategies for managing and preventing post-operative breakouts.
What is Laparoscopic Surgery?
Laparoscopic surgery, also known as minimally invasive surgery or keyhole surgery, is a surgical technique that allows surgeons to perform operations through small incisions (usually 0.5-1.5 cm) using a laparoscope, a thin fiber-optic instrument equipped with a light and camera. The laparoscope projects images of the inside of the abdomen or pelvis onto a screen, enabling the surgeon to visualize and operate on the internal organs without the need for a large incision.
Compared to traditional open surgery, laparoscopic surgery offers several benefits, including:
- Smaller incisions and scars
- Less post-operative pain and discomfort
- Reduced blood loss and risk of infection
- Shorter hospital stays and recovery times
- Quicker return to normal activities and work
Laparoscopic surgery is commonly used for a wide range of abdominal and pelvic procedures, including gallbladder removal, appendectomy, hernia repair, hysterectomy, and bariatric surgery.

Common Laparoscopic Procedures
Laparoscopic Cholecystectomy
Laparoscopic cholecystectomy, or gallbladder removal, is one of the most common laparoscopic procedures performed worldwide. The gallbladder is a small, pear-shaped organ located beneath the liver that stores and concentrates bile, a digestive fluid that helps break down fats. Gallstones, which are hardened deposits of bile, can form in the gallbladder and cause symptoms like abdominal pain, nausea, and vomiting. Laparoscopic cholecystectomy is typically recommended when gallstones cause recurrent symptoms or complications like inflammation or infection of the gallbladder (cholecystitis).
During a laparoscopic cholecystectomy, the surgeon makes four small incisions in the abdomen and inserts the laparoscope and surgical instruments. The gallbladder is carefully separated from the liver and other surrounding structures, and then removed through one of the incisions. Most patients can go home the same day or the following morning and resume normal activities within a week or two.
Laparoscopic Appendectomy
The appendix is a small, finger-shaped pouch attached to the colon in the lower right abdomen. While its exact function is unclear, the appendix can become inflamed or infected, a condition known as appendicitis. Appendicitis is a medical emergency that requires prompt surgical removal of the appendix to prevent rupture and potentially life-threatening complications like peritonitis (infection of the abdominal lining).
Laparoscopic appendectomy has become the preferred approach for treating appendicitis in most cases. The surgeon makes three small incisions in the abdomen and uses the laparoscope and instruments to visualize, dissect, and remove the inflamed appendix. Compared to open appendectomy, laparoscopic appendectomy is associated with less post-operative pain, shorter hospital stays, and faster recovery times.
Laparoscopic Hernia Repair
A hernia occurs when an internal organ or tissue protrudes through a weak spot in the surrounding muscle or connective tissue. Hernias can develop in various locations, but the most common types are inguinal (groin), umbilical (belly button), and incisional (at the site of a previous surgery). Hernias may cause a visible bulge, pain, or discomfort, and can lead to complications like incarceration (trapped tissue) or strangulation (cut-off blood supply to the tissue).
Laparoscopic hernia repair is a minimally invasive technique that involves placing a mesh patch over the hernia defect to reinforce the weakened area. The surgeon makes three to four small incisions in the abdomen and uses the laparoscope and instruments to visualize and repair the hernia from the inside. Laparoscopic hernia repair is associated with less post-operative pain and faster recovery compared to open hernia repair, and may be particularly beneficial for patients with bilateral (both sides) or recurrent hernias.
Laparoscopic Hysterectomy
A hysterectomy is a surgical procedure to remove the uterus, and sometimes the ovaries and fallopian tubes as well. Hysterectomy may be recommended for various conditions, including uterine fibroids, endometriosis, pelvic support problems, abnormal uterine bleeding, and gynecologic cancers. Laparoscopic hysterectomy is a minimally invasive approach that involves removing the uterus through small incisions in the abdomen, rather than a large incision as in traditional open hysterectomy.
There are several types of laparoscopic hysterectomy, depending on the extent of removal and the specific technique used:
- Total laparoscopic hysterectomy (TLH): The entire uterus and cervix are removed through the laparoscopic incisions.
- Laparoscopic supracervical hysterectomy (LSH): The upper part of the uterus is removed, while the cervix is left in place.
- Laparoscopic-assisted vaginal hysterectomy (LAVH): The uterus is detached laparoscopically and then removed through the vagina.
- Robotic-assisted laparoscopic hysterectomy: The surgeon uses a robotic system to control the laparoscopic instruments and perform the hysterectomy.
Compared to open hysterectomy, laparoscopic hysterectomy is associated with less blood loss, shorter hospital stays, and quicker recovery times. However, not all patients are candidates for laparoscopic hysterectomy, depending on factors like uterine size, prior surgeries, and the reason for the hysterectomy.
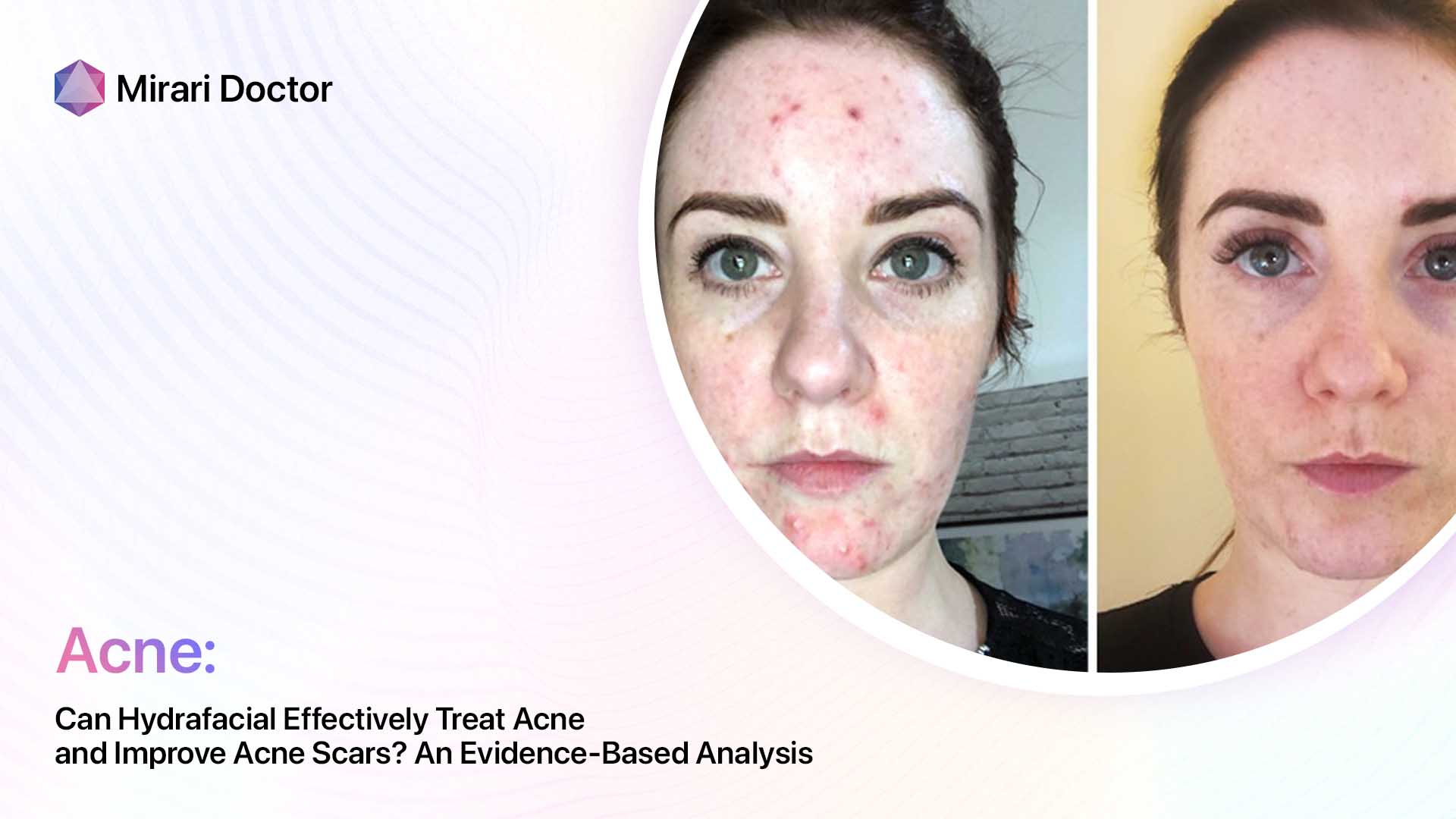
Acne: An Overview
Acne is a common skin condition that occurs when hair follicles become clogged with oil and dead skin cells. Acne can manifest as various types of lesions, including:
- Whiteheads (closed comedones)
- Blackheads (open comedones)
- Papules (small, red, raised bumps)
- Pustules (papules with pus at the tip)
- Nodules (large, solid, painful lumps beneath the surface of the skin)
- Cysts (painful, pus-filled lumps beneath the surface of the skin)
Acne most commonly affects the face, neck, chest, back, and shoulders, where sebaceous glands are most concentrated. While acne is most common during adolescence due to hormonal changes, it can affect people of all ages and persist into adulthood.

What Causes Acne?
Acne develops when hair follicles become plugged with oil and dead skin cells. Several factors can contribute to this process, including:
- Excess sebum production: Sebaceous glands secrete an oily substance called sebum to lubricate and protect the skin. When too much sebum is produced, it can combine with dead skin cells and clog hair follicles.
- Hormonal changes: Androgens, male hormones present in both males and females, stimulate sebum production. Hormonal fluctuations during puberty, menstrual cycles, pregnancy, and menopause can trigger or worsen acne.
- Bacterial growth: Propionibacterium acnes (P. acnes), a bacteria that normally lives on the skin, can proliferate in clogged hair follicles and contribute to inflammation and acne lesions.
- Inflammation: When hair follicles become clogged and bacteria multiply, the immune system may respond with inflammation, leading to redness, swelling, and the formation of acne lesions.
- Genetics: Acne tends to run in families, suggesting a genetic predisposition to the condition.
- Certain medications: Some drugs, such as corticosteroids, testosterone, and lithium, can trigger or worsen acne.
- Diet: While the relationship between diet and acne is complex and not fully understood, some studies suggest that certain foods, such as high-glycemic-index carbohydrates and dairy products, may exacerbate acne in some individuals.
Types of Acne
Acne can be classified into two main categories based on the type and severity of lesions:
- Non-inflammatory acne: This type of acne consists of comedones (whiteheads and blackheads) that are not associated with significant inflammation or redness. Non-inflammatory acne is typically mild and can often be managed with over-the-counter topical treatments and good skincare habits.
- Inflammatory acne: This type of acne involves papules, pustules, nodules, and cysts that are red, swollen, and often painful. Inflammatory acne is more severe and may require prescription-strength topical or oral medications to control. If left untreated, inflammatory acne can lead to scarring and post-inflammatory hyperpigmentation.
In addition to these main categories, acne can be further classified based on severity:
- Mild acne: Characterized by a few scattered comedones, papules, and pustules, with no nodules or cysts.
- Moderate acne: Characterized by more numerous comedones, papules, and pustules, with some nodules and cysts.
- Severe acne: Characterized by extensive comedones, papules, pustules, nodules, and cysts, often with scarring and inflammation.
Acne Triggers
In addition to the underlying causes of acne, various factors can trigger or worsen breakouts in susceptible individuals. Common acne triggers include:
- Hormonal fluctuations: Changes in hormone levels during puberty, menstrual cycles, pregnancy, and menopause can stimulate sebum production and lead to breakouts.
- Stress: Stress can increase cortisol levels, which can stimulate sebum production and exacerbate acne.
- Certain medications: Drugs like corticosteroids, testosterone, lithium, and some oral contraceptives can trigger or worsen acne.
- Diet: High-glycemic-index foods and dairy products have been associated with acne in some studies, although more research is needed to confirm these links.
- Cosmetics and skincare products: Comedogenic (pore-clogging) makeup, sunscreen, and moisturizers can contribute to acne, especially if not removed properly.
- Environmental factors: High humidity, pollution, and exposure to irritants like oils and greases can worsen acne.
- Friction and pressure: Rubbing, squeezing, or picking at acne lesions, as well as friction from helmets, hats, or tight collars, can irritate the skin and exacerbate breakouts.
Identifying and avoiding personal acne triggers can be an important part of managing and preventing breakouts.

The Link Between Laparoscopic Surgery and Acne
While acne is not typically listed as a common side effect of laparoscopic surgery, some patients do report experiencing new or worsening breakouts in the weeks following their procedure. The exact link between laparoscopic surgery and acne is not well understood, but several theories have been proposed based on case reports and small studies.
Case Reports and Studies
A few case reports and small studies have described patients developing acne or acne-like rashes after undergoing laparoscopic surgery, particularly laparoscopic bariatric procedures like sleeve gastrectomy and gastric bypass.
In a case series published in the journal Obesity Surgery, four patients developed a diffuse acneiform eruption 2-4 weeks after undergoing laparoscopic sleeve gastrectomy. The rash was characterized by multiple erythematous papules and pustules on the face, chest, back, and upper arms. Skin biopsies revealed a neutrophilic folliculitis, consistent with an acne-like eruption. The authors proposed that the rash may be due to post-operative changes in gut microbiota leading to increased levels of circulating androgens and sebum production.
Another case report, published in the Journal of the American Academy of Dermatology, described a similar acneiform eruption in a patient after laparoscopic gastric bypass surgery. The authors suggested that the rash may be related to post-operative nutritional deficiencies or hormonal changes.
While these reports suggest a potential link between laparoscopic bariatric surgery and acne, it’s important to note that they are based on a small number of cases and may not be representative of the general population. More research is needed to determine the prevalence and underlying mechanisms of post-operative acne in patients undergoing laparoscopic surgery.
Proposed Mechanisms
Several mechanisms have been proposed to explain the potential link between laparoscopic surgery and acne, although more research is needed to confirm these hypotheses:
- Hormonal changes: Laparoscopic surgery, particularly bariatric procedures, can lead to rapid weight loss and changes in hormone levels. Rapid weight loss has been associated with increased levels of circulating androgens, which can stimulate sebum production and contribute to acne. Additionally, some studies have suggested that the stress of surgery itself may lead to hormonal fluctuations that could trigger breakouts.
- Nutritional deficiencies: Laparoscopic bariatric surgery can lead to nutritional deficiencies due to reduced food intake and impaired absorption of nutrients. Deficiencies in vitamins A, D, E, and zinc have been associated with acne in some studies. However, the link between post-operative nutritional deficiencies and acne remains speculative.
- Changes in gut microbiota: Laparoscopic bariatric surgery can lead to changes in the gut microbiome due to altered food intake and digestive anatomy. Some researchers have proposed that these changes in gut bacteria may influence the skin microbiome and contribute to acne. However, more research is needed to understand the complex relationship between the gut-skin axis and acne.
- Medications: Some medications commonly used during and after laparoscopic surgery, such as antibiotics and corticosteroids, have been associated with acne in some patients. However, the risk of medication-induced acne is generally low and resolves after discontinuing the drug.
It’s important to note that these proposed mechanisms are based on limited evidence and require further investigation. The link between laparoscopic surgery and acne may be multifactorial and vary depending on the individual patient and type of procedure.

Acne After Specific Laparoscopic Procedures
The risk and prevalence of acne after laparoscopic surgery may vary depending on the specific procedure and patient factors. Let’s take a closer look at acne after some common laparoscopic procedures:
Acne After Laparoscopic Cholecystectomy
Laparoscopic cholecystectomy, or gallbladder removal, is one of the most common laparoscopic procedures performed worldwide. While acne is not a widely reported side effect of laparoscopic cholecystectomy, some patients may experience skin changes or breakouts due to post-operative hormonal fluctuations or stress.
In a study published in the Journal of the Society of Laparoendoscopic Surgeons, researchers found that patients undergoing laparoscopic cholecystectomy had higher levels of stress hormones like cortisol and adrenaline compared to those undergoing open cholecystectomy. These hormonal changes could potentially contribute to acne in susceptible individuals.
However, the overall risk of developing acne after laparoscopic cholecystectomy appears to be low based on the available evidence. More research is needed to determine the prevalence and risk factors for post-cholecystectomy acne.
Acne After Laparoscopic Appendectomy
Laparoscopic appendectomy is a common emergency procedure for treating appendicitis. While skin complications like surgical site infections and allergic reactions to antiseptics have been reported after laparoscopic appendectomy, acne is not a widely recognized side effect.
A few case reports have described patients developing acne or acne-like rashes after laparoscopic appendectomy, but these appear to be rare and isolated incidents. In one case, a patient developed a generalized acneiform eruption after laparoscopic appendectomy, which the authors attributed to post-operative antibiotic use.
Given the lack of large-scale studies or systematic reviews on the topic, the risk of developing acne after laparoscopic appendectomy remains unclear. More research is needed to determine if there is a significant association between this procedure and post-operative acne.
Acne After Laparoscopic Hernia Repair
Laparoscopic hernia repair is a minimally invasive technique for treating various types of hernias, including inguinal, umbilical, and incisional hernias. While wound complications and mesh infections are well-documented risks of laparoscopic hernia repair, acne is not a commonly reported side effect.
A search of the literature did not yield any specific case reports or studies on acne after laparoscopic hernia repair. However, some patients may experience skin irritation or rashes due to the adhesive dressings or mesh materials used during the procedure.
If you develop any unusual skin symptoms after laparoscopic hernia repair, it’s important to follow up with your surgeon or a dermatologist for evaluation and management.
Acne After Laparoscopic Hysterectomy
Laparoscopic hysterectomy is a minimally invasive surgical procedure for removing the uterus and sometimes the ovaries and fallopian tubes. While skin complications like surgical site infections and allergic reactions have been reported after laparoscopic hysterectomy, acne is not a widely recognized side effect.
However, some patients may experience hormonal changes after hysterectomy that could potentially contribute to acne, particularly if the ovaries are also removed. Removal of the ovaries leads to a sudden decrease in estrogen and progesterone levels, which can trigger a temporary flare-up of acne in some women.
A few studies have reported an increased prevalence of acne and other skin conditions like hirsutism (excessive hair growth) in women who have undergone surgical menopause due to bilateral oophorectomy (removal of both ovaries). However, these studies were not specific to laparoscopic hysterectomy and may not be generalizable to all patients.
If you experience new or worsening acne after laparoscopic hysterectomy, it’s important to discuss your concerns with your gynecologist or a dermatologist. They can help determine if your acne may be related to post-operative hormonal changes and recommend appropriate treatment options.

The Role of Anesthesia in Post-Operative Acne
Some patients have raised concerns about the potential link between general anesthesia and post-operative acne. While there is limited evidence to suggest a direct causal relationship between anesthesia and acne, some studies have proposed potential mechanisms by which anesthesia could contribute to skin changes or breakouts.
One theory is that the stress of surgery and anesthesia may lead to hormonal fluctuations that could trigger acne in susceptible individuals. Anesthesia has been shown to increase levels of stress hormones like cortisol and adrenaline, which can stimulate sebum production and inflammation in the skin.
Another proposed mechanism is that the medications used during anesthesia, such as opioids and benzodiazepines, may have immunomodulatory effects that could disrupt the skin’s natural defenses against acne-causing bacteria. However, this hypothesis remains speculative and requires further investigation.
It’s important to note that the risk of developing acne after general anesthesia appears to be low based on the available evidence. Most studies on the topic have been small, retrospective, and not specific to laparoscopic surgery. More research is needed to determine if there is a significant association between anesthesia and post-operative acne.
If you have a history of acne or are concerned about the potential effects of anesthesia on your skin, it’s important to discuss your concerns with your anesthesiologist and surgeon before your procedure. They can help assess your individual risk factors and recommend strategies for minimizing the risk of post-operative skin complications.
Managing Acne After Laparoscopic Surgery
If you develop new or worsening acne after laparoscopic surgery, there are several strategies you can use to manage your symptoms and promote clearer, healthier-looking skin. Here are some tips for managing post-operative acne:
Gentle Skincare
One of the most important steps in managing post-operative acne is to practice gentle, non-irritating skincare. This means avoiding harsh scrubs, exfoliants, and astringents that can further irritate the skin and worsen inflammation.
Instead, opt for a mild, fragrance-free cleanser that won’t strip the skin of its natural oils. Look for products that are labeled “non-comedogenic” or “oil-free,” as these are less likely to clog pores and exacerbate acne.
After cleansing, apply a light, non-greasy moisturizer to keep the skin hydrated and support its natural barrier function. If your skin is particularly dry or sensitive, you may also benefit from a moisturizer containing ceramides or hyaluronic acid.
Be sure to remove all makeup and sunscreen before going to bed, and avoid touching or picking at your acne lesions, as this can introduce bacteria and cause further inflammation.

Topical Treatments
If your post-operative acne is mild to moderate, you may be able to manage your symptoms with over-the-counter topical treatments. Look for products containing the following active ingredients:
- Benzoyl peroxide: This antimicrobial agent helps kill acne-causing bacteria and unclog pores. It’s available in various strengths and formulations, including cleansers, creams, and gels.
- Salicylic acid: This beta-hydroxy acid (BHA) helps exfoliate the skin and unclog pores. It’s commonly found in acne washes, toners, and spot treatments.
- Retinoids: These vitamin A derivatives help regulate cell turnover and reduce inflammation. Over-the-counter retinoids like adapalene (Differin) are available in lower strengths than prescription retinoids.
When using topical acne treatments, it’s important to start slowly and gradually increase the frequency and strength of application to minimize the risk of irritation. Be sure to follow the product instructions carefully and discontinue use if you experience persistent redness, dryness, or peeling.
If your acne is severe or not responding to over-the-counter treatments, your dermatologist may recommend prescription-strength topical medications like tretinoin, tazarotene, or clindamycin.

Oral Medications
For more severe or persistent cases of post-operative acne, your dermatologist may recommend oral medications to help control your symptoms. Some common oral acne medications include:
- Antibiotics: Oral antibiotics like doxycycline and minocycline can help reduce inflammation and kill acne-causing bacteria. They are typically used for short-term treatment of moderate to severe acne.
- Hormonal therapies: For women with hormone-related acne, oral contraceptives and anti-androgen medications like spironolactone can help regulate hormone levels and reduce sebum production.
- Isotretinoin: This oral retinoid is reserved for severe, nodular acne that has not responded to other treatments. Isotretinoin is highly effective but requires close monitoring due to potential side effects like dry skin, lips, and eyes, as well as birth defects if taken during pregnancy.
Your dermatologist will determine if oral acne medications are appropriate for your individual case based on factors like the severity of your acne, medical history, and potential contraindications.
Lifestyle Modifications
In addition to medical treatments, certain lifestyle modifications may help manage and prevent post-operative acne flare-ups. These include:
- Stress management: Engaging in stress-reducing activities like deep breathing, meditation, yoga, or exercise may help regulate stress hormones and reduce inflammation in the skin.
- Diet modifications: While the relationship between diet and acne is complex, some studies suggest that limiting high-glycemic-index foods and dairy products may be beneficial for some patients with acne-prone skin.
- Sun protection: Using a non-comedogenic, broad-spectrum sunscreen with at least SPF 30 can help protect the skin from UV damage and reduce the risk of post-inflammatory hyperpigmentation.
- Avoiding irritants: Minimizing exposure to potential acne triggers like heavy makeup, greasy hair products, and tight-fitting clothing or equipment may help reduce the risk of breakouts.
Remember, everyone’s skin is unique, and what works for one person may not work for another. It may take some trial and error to find the right combination of treatments and lifestyle modifications to manage your post-operative acne.

When to See a Dermatologist
If you develop new or worsening acne after laparoscopic surgery, it’s important to know when to seek professional help. You should consider making an appointment with a dermatologist if:
- Your acne is severe, painful, or not responding to over-the-counter treatments after 4-6 weeks of consistent use.
- Your acne is causing significant scarring or post-inflammatory hyperpigmentation.
- Your acne is affecting your self-esteem, mental health, or quality of life.
- You suspect your acne may be related to a medication or underlying medical condition.
- You have a history of severe or cystic acne and are concerned about a post-operative flare-up.
A dermatologist can provide a comprehensive evaluation of your skin and recommend personalized treatment options based on the type and severity of your acne, as well as your individual needs and preferences. They can also monitor your progress and adjust your treatment plan as needed to help you achieve clearer, healthier-looking skin.
Preventing Post-Operative Acne Flare-Ups
While not all cases of post-operative acne can be prevented, there are some steps you can take to minimize your risk of developing breakouts after laparoscopic surgery:
- Discuss your acne history with your surgeon before the procedure. If you have a history of acne or are concerned about post-operative breakouts, let your surgeon know before your procedure. They may be able to recommend prophylactic measures or refer you to a dermatologist for pre-operative skincare guidance.
- Maintain a gentle, non-irritating skincare routine before and after surgery. Avoiding harsh skincare products and practices can help minimize inflammation and reduce the risk of post-operative acne flare-ups. Stick to a mild cleanser, fragrance-free moisturizer, and non-comedogenic sunscreen.
- Manage stress before and after surgery. Engaging in stress-reducing activities like deep breathing, meditation, or gentle exercise can help regulate stress hormones and reduce inflammation in the skin. If you’re feeling overwhelmed or anxious about your surgery, don’t hesitate to reach out to your healthcare team or a mental health professional for support.
- Follow your surgeon’s post-operative instructions carefully. Adhering to your surgeon’s guidelines for incision care, activity restrictions, and medication use can help minimize the risk of complications and promote optimal healing. If you have any questions or concerns about your post-operative care, don’t hesitate to ask your surgeon or a member of your healthcare team.
- Avoid potential acne triggers during your recovery. Minimizing exposure to potential acne triggers like heavy makeup, greasy hair products, and tight-fitting clothing or equipment may help reduce the risk of post-operative breakouts. If you’re taking any new medications or supplements after surgery, ask your doctor if they could potentially contribute to acne.
Remember, everyone’s skin is unique, and not all cases of post-operative acne can be prevented. If you do develop breakouts after laparoscopic surgery, don’t hesitate to reach out to your surgeon or a dermatologist for guidance and support.
Frequently Asked Questions
Is acne a common side effect of laparoscopic surgery?
While acne is not typically listed as a common side effect of laparoscopic surgery, some patients do report experiencing new or worsening breakouts after their procedure. The exact prevalence of post-operative acne is not well established and may vary depending on the type of surgery and individual patient factors.
Can laparoscopic surgery cause hormonal changes that trigger acne?
Some studies have suggested that the stress of surgery and anesthesia may lead to hormonal fluctuations that could potentially trigger acne in susceptible individuals. Additionally, certain laparoscopic procedures like bariatric surgery and hysterectomy with oophorectomy can cause more significant hormonal changes that may contribute to acne. However, more research is needed to fully understand the relationship between laparoscopic surgery, hormones, and acne.
How long does post-operative acne typically last?
The duration of post-operative acne can vary depending on the individual and the underlying cause of the breakouts. In some cases, acne may resolve on its own within a few weeks to months after surgery as the body adjusts to post-operative changes. However, some patients may experience more persistent acne that requires medical treatment.
Can I use my regular acne treatments after laparoscopic surgery? If you have a pre-existing acne treatment regimen, it’s important to discuss its safety and appropriateness with your surgeon and dermatologist in the context of your post-operative care. Some acne medications, particularly oral antibiotics and retinoids, may interact with other medications or affect wound healing. Your healthcare team can provide personalized guidance on how to safely manage your acne after surgery.
When should I see a dermatologist for post-operative acne? You should consider making an appointment with a dermatologist if your post-operative acne is severe, painful, or not responding to over-the-counter treatments after 4-6 weeks of consistent use. Additionally, if your acne is causing significant scarring, hyperpigmentation, or emotional distress, or if you suspect it may be related to a medication or underlying medical condition, it’s important to seek professional evaluation and care.
Conclusion
Acne after laparoscopic surgery is a potential side effect that can be concerning and frustrating for patients. While the exact link between laparoscopic procedures and post-operative breakouts is not well understood, several factors like hormonal changes, stress, and medications may play a role.
If you develop new or worsening acne after laparoscopic surgery, it’s important to practice gentle skincare, consider over-the-counter or prescription acne treatments, and make lifestyle modifications that support skin health. If your acne is severe or not responding to self-care measures, don’t hesitate to seek evaluation and guidance from a dermatologist.
Remember, everyone’s skin and post-operative journey is unique. By working closely with your healthcare team and prioritizing self-care, you can navigate the challenges of post-operative acne and work towards clearer, healthier-looking skin.
References
- Adelman, M., Munro, C., & Stetson, C. L. (2022). Acne Vulgaris. In StatPearls. StatPearls Publishing.
- Alhetheli, G. I. (2019). Acne vulgaris: Perceptions and beliefs of Saudi adolescent males. Journal of Family & Community Medicine, 26(1), 27-32.
- Bhate, K., & Williams, H. C. (2013). Epidemiology of acne vulgaris. The British Journal of Dermatology, 168(3), 474-485.
- Bowe, W. P., & Logan, A. C. (2011). Acne vulgaris, probiotics and the gut-brain-skin axis – back to the future? Gut Pathogens, 3(1), 1.
- Dréno, B. (2017). What is new in the pathophysiology of acne, an overview. Journal of the European Academy of Dermatology and Venereology, 31 Suppl 5, 8-12.
- Hazarika, N., & Archana, M. (2016). The Psychosocial Impact of Acne Vulgaris. Indian Journal of Dermatology, 61(5), 515-520.
- Juhl, C. R., Bergholdt, H., Miller, I. M., Jemec, G., Kanters, J. K., & Ellervik, C. (2018). Dairy Intake and Acne Vulgaris: A Systematic Review and Meta-Analysis of 78,529 Children, Adolescents, and Young Adults. Nutrients, 10(8), 1049.
- Kraft, J., & Freiman, A. (2011). Management of acne. CMAJ : Canadian Medical Association Journal, 183(7), E430-E435.
- Marson, J. W., & Baldwin, H. E. (2019). An Overview of Acne Therapy, Part 1: Topical therapy, Oral Antibiotics, Laser and Light Therapy, and Dietary Interventions. Dermatologic Clinics, 37(2), 183-193.
- Marson, J. W., & Baldwin, H. E. (2019). An Overview of Acne Therapy, Part 2: Hormonal Therapy and Isotretinoin. Dermatologic Clinics, 37(2), 195-203.
- Rocha, M. A., & Bagatin, E. (2018). Adult-onset acne: prevalence, impact, and management challenges. Clinical, Cosmetic and Investigational Dermatology, 11, 59-69.
- Sutaria, A. H., Masood, S., & Schlessinger, J. (2022). Acne Vulgaris. In StatPearls. StatPearls Publishing.
- Tanghetti, E. A., Kawata, A. K., Daniels, S. R., Yeomans, K., Burk, C. T., & Callender, V. D. (2014). Understanding the burden of adult female acne. The Journal of Clinical and Aesthetic Dermatology, 7(2), 22-30.
- Zaenglein, A. L., Pathy, A. L., Schlosser, B. J., Alikhan, A., Baldwin, H. E., Berson, D. S., Bowe, W. P., Graber, E. M., Harper, J. C., Kang, S., Keri, J. E., Leyden, J. J., Reynolds, R. V., Silverberg, N. B., Stein Gold, L. F., Tollefson, M. M., Weiss, J. S., Dolan, N. C., Sagan, A. A., . . . Bhushan, R. (2016). Guidelines of care for the management of acne vulgaris. Journal of the American Academy of Dermatology, 74(5), 945-973.e33.
Related articles
Made in USA